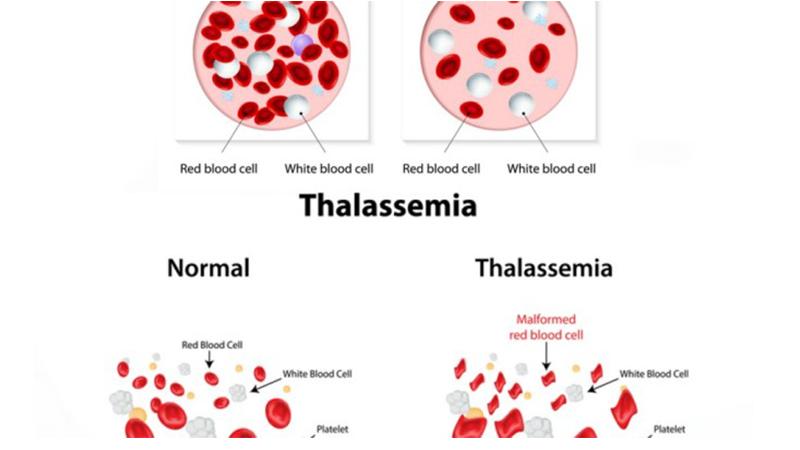
term thalassaemia is derived from the Greek word ‘thalassa’, which means “the sea” referring to the Mediterranean, and ‘emia’, meaning ‘related to blood. Thalassaemiascollectively known as haemoglobinopathies is a group of inherited blood disorderspassed down through families characterized by anomalies in the synthesis of globin chains of haemoglobin resulting in variable phenotypes ranging from clinically asymptomatic to severe anaemia.
Thalassaemia was first recognized by Thomas Cooley and Pearl Lee in 1925as a form of severe anaemia associated with splenomegaly and changes in bones amongchildren. Thalassaemia is one of themajor health problems,which links withimmense emotional, psychological and economic burden on millions of people around the world. Recent data indicates that around 5-7% of the world’s population is affectedby this inherited disorderand 300,000-500,000 children are born each year with the severe homozygous states; a severe form of thalassaemia.
Thalassaemias are autosomal recessive haemoglobinopathies characterized by defects in the production of globin polypeptide chains in the adult haemoglobin. This inherited disorder is one of the commonest encountered monogenic diseases documented. Different types of thalassaemias have been identified to date. Out of these, two major types of thalassaemias, alpha and beta, which have been named according to the defects in their protein chainsare commonly encountered. There are two main types of beta thalassaemias;thalassaemia major and thalassaemia minor. When defective genes are inherited from either of the parents it is named as thalassaemiaminor (homozygous). If defective genes are inherited from both parents, the disease is called thalassaemia major (heterozygous), and affected individuals fail to maintain the required levels of haemoglobin.
Infections transmitted via frequent blood transfusions are well documented among thalassaemicpatients. However, modernizations in blood transfusion methodologies and meticulous donor screening programshave minimized the transfusion related infections by greatextent. Life-threatening non-transfusion related infections have been documented in beta thalassaemic patients in comparison to that of the healthy population. Infections rank the second most common cause of mortality and morbidity in beta thalassaemia major patients to date.
Many alterations in the body’s immune system in beta thalassaemia major patients have been documented. Arguably, in the lack of evidence-based data on a direct relationship between defects in the immune system and the predisposition to severe infections in beta thalassaemia major patients, it is always a challenge for clinicians to arrive at an early definitive diagnosis and prevent further complications.
In the past, beta thalassaemia used to be a paediatric disease. Thanks to the implementation of upgraded management strategies for beta thalassaemic patients,the median age of this cohortof patients has been improved immensely (Figure 1). Improved life expectancy has not only beenseen in European and Mediterranean countries, but such changes have been reported in most Asian countries as well. This is largely due to better management approaches, particularly wide usage of iron chelating therapy, genetic counseling, awareness, population screening, and the availability of prenatal diagnosis, most beta thalassaemic patients celebrate their 45-50th birthdays.Recent developments and the discovery of advanced treatment approaches, beta thalassaemia patients are seeing a better hope for future; notably through bone marrow transplantation, gene therapy, and stem cell therapy.
After the successful elimination of the leading causes of deaths of beta thalassaemic patients over the last decade, patients have now confrontedwith a novel fatal challenge;infections. For the last decade, other than the commonmicrobial agents, uncommon infectious agents have also been identified in beta thalassaemic patients. It is estimated that infectionsare the second highest cause of death among beta thalassaemic patients. An improved life span of these patients by 2-3 decades has made this cohort of thepatientfurther vulnerable to infections.
Figure 1. Comparison of life expectancy of beta thalassaemics. Comparison of life expectancy for patients who were alive at the beginning of 1970, 1980, 1990 and 2000, based on mortality in the subsequent five years (four years for the period 2000–2003) Reproduced from Modell et al. 2008.
Since the identification of beta thalassaemia major, themedical and scientific communities have acquired a plethora of information on this autosomal recessive haemoglobinopathy over the next eight decades. It was initially thought that the diseasewas confined to the Mediterranean region. However, subsequent studies indicated that beta thalassaemia has been detected outside the Mediterranean basin particularly in tropical countries where malaria is endemic. But, due to mass population migrations and intermarriage between different ethnic groups, thalassaemia has been introduced to almost every country. As a result, beta thalassaemia is reported and documented in all parts of the world.
In the 1950s, anaemia was the leading cause of death of beta thalassaemia major patients. However, the pendulum shifted and iron overloadtopped the list the causes of death over the next four decades, until the mid 1990s. The introductions of iron chelating agents revolutionisedthe management of beta thalassaemiaand havesuccessfully eliminated the risk of iron overlord. Recommendations of packed red cells havefurther reduced deaths that resulted incardiac failure to considerable levels.
Once the leading causes of death among beta thalassaemicmajor patients have been eliminated over the last decade, these patients are now confronted with a new fatal challenge;life threatening infections. For the last decade other than common microbial agents, an uncommon presentation of common infectious diseases, and more importantly novel infectious agents that have never been identified in beta thalassaemic patientswere detected. To date, infections are ranked as the second most common cause of mortality and morbidity in beta thalassaemia major patients.
These developments have proved to be an intense challenge for cliniciansarriving at an early and definitive diagnosis, and the prevention of complications following infectious, and has forced specialised clinicians to revise the management guidelines forthalassaemic major patients, giving more weight to the clinical management aspects on infections.
A number of anatomical and unique physiological defects have been identified among beta thalassaemic major patients, which unduly predispose this cohort of patients for infections. It was coined that beta thalassaemic major patients were immunocompromised. It is true thatnumberof pathological changes have been detected among beta thalassaemic major patients, which predisposethemfor infections. Update documented data reveal that all beta thalassaemic majorpatients are born without “recognisable” defects in the immune system.
A number of predisposed factors thatpossibly predispose betathalassaemics for life threatening infections have been identified; severe anaemia, iron overload andsplenectomy.
Advancement in molecular medicine has revolutionised the laboratory diagnostic approachesin the field infections diseases. Different molecular diagnosis platforms such as PCR, gene sequence, MALDI-TOF®,VITEK 2®,array techniquesand gene probes have allowed microbiologist to arrive at a definitive identification of infectious agents with high accuracy when compared to the past where most of the identifications were based either on phenotypical or biochaemical characters of the microorganisms, which had a number of limitations. These technological advances have not only allowed biomedical scientists to detect the infectious agents promptly and more accurately
Beta thalassaemic patients are at a greater risk of contracting non-transfusion dependent infections when compared to healthy individuals. It is clear that splenectomy, iron overload and suppression of the immune system have predisposed beta thalassaemicmajor patients tonon-transfusion dependent infections.
Apart from these multifactorial causes, its believe that an improved life expectancy has predisposed them to life threatening infection. However, documented case reports suggest that other unidentified pathological changes might lead them to be susceptible to life threatening infections. This underscored importance of systematic approach tointerdisciplinary research,increases usage of vaccines and the rational usage of antibiotics to combat life threatening infections which are essential to reduce mortality and morbidity of beta thalassaemicmajor patents, while implementation of genetic counseling, awareness, population screening, discouragement of consanguinity, and the availability of prenatal diagnosis reduces the number of beta thalassaemicmajor births.
(Part of this essay submitted for school EPQ/Crest award projects).
This is the summery of young writer Himath Perera’s A/L science project (Lyceum International School, Wattala), which he has collaborated with Prof Anuja Premawadrana ( Consultant VP) and Dr. S. Mettananda (Consultant Paediatrician); both are experts in the field of thalassaemia and both attached to Faculty of Medicine Ragama.
Perera did an extensive Pubmed research study on thalassaemia with infections as part of this A/L science project.
