This is Cerebral Palsy (CP) awareness month: Lankans diagnosed with this condition exceed some western countries
 Cerebral Palsy (CP) is the most common physical disability in children which affects movement and posture. It is a neurological disorder caused by a non-progressive brain injury or malformation that occurs while the child’s brain is still developing. There is no single cause for Cerebral Palsy and no new scientifically proven method has been found yet to totally prevent or cure cerebral palsy.
Cerebral Palsy (CP) is the most common physical disability in children which affects movement and posture. It is a neurological disorder caused by a non-progressive brain injury or malformation that occurs while the child’s brain is still developing. There is no single cause for Cerebral Palsy and no new scientifically proven method has been found yet to totally prevent or cure cerebral palsy.
On the upside, Cerebral Palsy is now emerging from the closet in which it was once hidden, largely due to the stigma surrounding it. More people are now talking about it; more parents are bringing children with suspected symptoms for early examination. This is largely due to the awareness raising efforts of the Health Ministry and a few private non government organizations such as, the Cerebral Palsy Lanka Foundation.
To get better insights into this still little understood neurological condition that largely affects children, the Sunday Observer spoke to Chartered Physiotherapist Dr Gopi Kitnasamy, Chairman and Founder of the Cerebral Palsy Lanka Foundation, the only one of its kind set up to cater solely to all the needs of a child afflicted by CP, under one roof.
In our interview, Dr Kitnasamy reiterated that while CP is not curable or preventable, it has been scientifically proved that early diagnosis of the condition will maximize a child’s mobility and potential . He lamented that, diagnosis for various reasons, is often delayed, impeding a child’s development growth ,which proper therapy and rehabilitation treatment offer.
Excerpts of the interview:
 Q. This is Cerebral Palsy Awareness month. Why is it a health issue that an entire month is dedicated to raising awareness about it?
Q. This is Cerebral Palsy Awareness month. Why is it a health issue that an entire month is dedicated to raising awareness about it?
A. Cerebral Palsy (CP) is the commonest physical disability in children, and affects the movement and posture. It is important to diagnose CP as soon as possible to maximize a child’s mobility and potential. Unfortunately, diagnosis is often delayed for a number of reasons.
Q. How many people are afflicted by this condition globally?
A. There are 17 million (estimated number) people across the world living with cerebral palsy. Another 350 million people are closely connected to a child or adult with CP, 4 in 1,000 births are diagnosed with CP.
Q. How many Lankans have this condition?
A. We are currently working on the statistics and estimate that there are more than 40,000 children and adults with CP in Sri Lanka. In Australia (similar population like us), there are 34,000 registered people with CP.
Q. In Sri Lanka, what districts have the highest incidence of CP?
A. According to data from our wheelchair and awareness camps, the Northern Province, particularly Jaffna district has the highest number, but we need to do further study to get the exact statistics.
 Q. Who are most at risk of developing this condition? Why?
Q. Who are most at risk of developing this condition? Why?
A. Premature babies, multiple births, infection during pregnancy, mothers with medical conditions, complicated deliveries, severe jaundice and seizures in infants are some of the factors that may increase a baby’s risk of being born with cerebral palsy.
Q. Is CP a ‘hidden’ problem?
A. Like other conditions, the severity can vary from very mild to very severe. Sometimes, the mild ones go unnoticed. And with the social stigma, many children with CP are kept housebound, so you don’t see them often in the society.
Q. How and when does CP begin developing in the human body? In the mother’s womb? Or after birth?
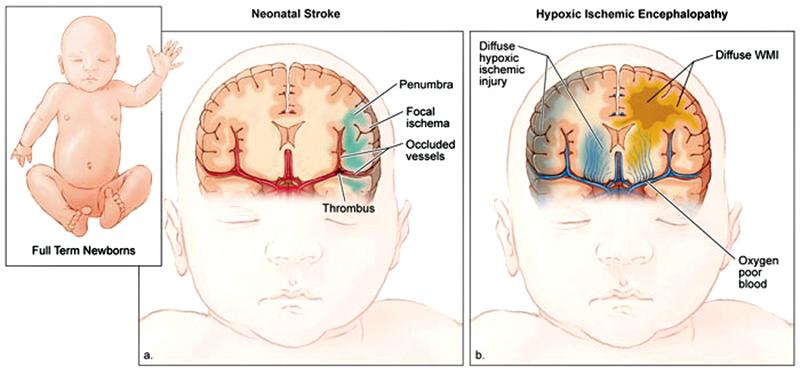
A. Timing, when the brain damage occurs to the developing brain, is an important component of a CP diagnosis. It can also impact the severity and type of Cerebral Palsy a child develops. When a child has congenital CP, it means events that occurred during pregnancy or at birth. Although congenital CP may not be diagnosed immediately, the condition exists at birth and can be detected months or years later. Seventy percent of all cerebral palsy diagnoses are diagnosed as congenital. As we know, the brain continues to develop after birth. In cases of Acquired Cerebral Palsy, it is believed the child was born without the condition, but acquired the brain damage before the brain fully developed. Acquired CP is not inherited. Up to 10% of all cases of diagnosed CP are acquired.
Q. If a mother gives birth to a baby with CP will she always give birth to babies with this condition? What are the risk factors?
A. No, unless there are genetic contributions. Risk factors do not cause cerebral palsy. However, the presence of some risk factors may lead to an increased chance of a child being born with cerebral palsy. Some of the factors identified are :premature birth (less than 32 weeks)very low birth weight, blood clotting problems (thrombophilia) inability of the placenta to provide the developing foetus with oxygen and nutrients RH or A-B-O blood type incompatibility between mother and baby, infection of the mother with German measles or other viral diseases in early pregnancy, bacterial infection of the mother, foetus or baby, that directly or indirectly attacks the infant’s central nervous system, prolonged loss of oxygen during pregnancy or birthing process, or severe jaundice shortly after birth.
Q. Is CP hereditary?
A. Cerebral Palsy is not a hereditary condition. Some genetic contributions to obstetric risk factors include preterm birth, placental abruption, fetal growth restriction, chorioamnionitis, preeclampsia, and breech presentations. A recent study has identified the familial recurrence of athetoid type of Cerebral Palsy which is common in developing countries like Sri Lanka. We have seen several families with more than one child with CP in Sri Lanka.
Q. What are the early signs of CP?
A. The most common early signs are developmental delays in reaching key growth milestones, such as, rolling over, crawling, sitting, and walking. While in lifting or carrying, there can be variations in muscle tone, such as being either too stiff (spasticity or spastic) or too floppy. Sucking and feeding difficulties, difficulty in holding the head upright, excessive crying, lack of attention, favouring one hand over the other (stiffness on the other side) are the other common signs.
Q. Will early detection help to delay the progress of this condition?
A. Early diagnosis for CP hastens the onset of therapy and treatment, ultimately minimizing resultant impairments, preserving cognitive function, and allowing time for the child and parents to adjust. Unfortunately, diagnosis is often delayed for a number of reasons.
Q. What are the most negative impacts of CP as it progresses?
A. Cerebral palsy can affect a person’s posture, balance and ability to move, communicate, eat, sleep and learn. The parts of the body affected by CP, the level of severity and combination of symptoms can differ in each person. Contracture of the muscle tissue due to severe tightening of the muscle (spasticity), which can inhibit bone growth, cause bending of bones, and result in joint deformities, dislocations, and partial dislocations.
People with CP may experience uncontrolled or unpredictable movements, muscles can be stiff, weak or tight and in some cases people have shaky movements or tremors. People with severe cerebral palsy may also have difficulty with swallowing, which can cause problems and lead to pneumonia, breathing problems, head and neck control, bladder and bowel control, poor eating which can lead to malnutrition and have dental and digestive problems.
Q. What is the normal life expectancy of someone with CP?
A. Although there have been no general study of life expectancy in people with cerebral palsy, most children affected by CP live between 30 and 70 years, depending on the severity of the condition. In general, a child with a mild case of CP usually lives longer than a child with mobility and intellectual limitations.
Q. You are the Chairman of the Cerebral Palsy Foundation. What inspired you to form this Foundation?
A. Our son Danush has CP, he is a very intelligent child. He uses a wheelchair because of his condition. It was when we wanted to admit him to a school that we realized it’s not an easy task in Sri Lanka. We went from door to door but none of those schools were ready to take him. Many special schools refused straight away and many didn’t have even a wheelchair access. Then, we reluctantly admitted him to a special school near our home (as we didn’t have a choice) where he was neglected and ignored. This prompted us to start a center to help children with CP and their families.
Q. What are the goals of this Center?
A. To provide educational and therapeutic services of international standard to these children in all districts of Sri Lanka and provide all these services under one roof to help the families of these children. We created “The Dream” concept to achieve these goals and make it a reality.
Q. How do the activities you have at the center match those goals?
A. We provide special education with individualized educational plans using the local curriculum and all the necessary and appropriate therapies needed for these children.
Q. In retrospect how do you rate the success of the outcome of such activities at the CP Center?
A. As our interventions are focused on improving their quality of life, we are seeing very good improvements in their conditions. We also have introduced early identification and early intervention program for infants as the first two years of life is very critical and the brain’s response is much better.
Q. As a Chartered Physiotherapist, what is the role of physiotherapy in achieving your goals?
A. Physiotherapy is considered as the most important aspects of treating children with CP. But the approach should be holistic and multidisciplinary to get best results.
Q. Since children with CP are mostly confined to wheelchairs, you were able to develop a special wheelchair swing allowing them the right to benefit from play equipment in parks like other children. Do you plan to instal more of these in future?
A. We have installed one of those swings at the Viharamahadevi park in Colombo and another at the Lady Ridgeway Hospital. Now, we have designed and developed a wheelchair merry go round and a sea saw, which is available at our Rajagiriya center. Our dream is to make at least one park in each district an inclusive park by installing these special play equipment.
Q. What about other forms of recreation for children with CP?
A. We have introduced the wheelchair race, relay and recently the Boccia game at the center. Boccia is a specialized game for children with CP which is one of the paralympic games.
Q. Apart from your center at Colombo, do you plan to set up others in different parts of the country which would also offer all the services a CP child needs under one roof?
A. At present, in partnership with the MJF Charitable Foundation, we run 3 centers, Rajagiriya, Moratuwa and Ambalantota. We will be starting another center in Kiran, in the Batticaloa district. Our vision is to start at least one such center in each district of Sri Lanka.
Q. What are the new breakthroughs regarding detection, preventing and treating CP globally?
A. Accurate early diagnosis using General Movement Assessment, early interventions and identification of genetic factors are the latest breakthroughs. The General Movements Assessment is a non-invasive and cost-effective way to identify neurological issues which may lead to cerebral palsy and other developmental disabilities. The assessment can be completed from birth to 20 weeks of age.
Q. Are they available in Sri Lanka? Where?
A. In collaboration with the Sri Lanka College of Paediatricians, we organized the first GM training program in Sri Lanka. 38 health professionals from many districts of Sri Lanka participated in this program and got trained in this most reliable, time, cost-efficient and globally used tool to identify these children as early as possible.
Q. As a parent of a child with CP what is your message to other parents?
A. Accept the truth, learn and understand more about your child’s condition, focus on early interventions, be part of the intervention program, foster your child’s intellectual development, education is very important, never get discouraged, be part of parent support groups.
