As Sri Lanka moves towards lowering its Maternal Mortality rates and success in that endeavour has been universally praised by world health organisations, ending preventable maternal mortality from various forms of self harm inflicted on themselves by mothers during and immediately after pregnancy is still a subject of concern. Indepth analyses done over the years by the Maternal & Child Morbidity & Mortality Surveillance Unit of the Family Health Bureau, Ministry of Health bear evidence of this fact, which found that in certain vulnerable groups the tendency for attempted suicides by pregnant or recently delivered women is a persistent problem.
 National Program Manager, Maternal & Child Morbidity & Mortality Surveillance Unit, and Secretary of the Sri Lanka Medical Association Dr Kapila Jayaratne explains to the Sunday Observer the reasons which drive these women to such desperate action and underlines the urgency of putting in place interventions to fill the gaps that prevent safe motherhood.
National Program Manager, Maternal & Child Morbidity & Mortality Surveillance Unit, and Secretary of the Sri Lanka Medical Association Dr Kapila Jayaratne explains to the Sunday Observer the reasons which drive these women to such desperate action and underlines the urgency of putting in place interventions to fill the gaps that prevent safe motherhood.
Excerpts …
Q. Maternal mortality continues to be a public health priority in national and international communities. With Sri Lanka having one of the lowest maternal mortality rates in the world, is it a public health priority as in other countries? If so why?
A. Maternal mortality is a composite index of a country’s health infrastructure and the socio-economic status. If a country cannot safeguard at least the health of pregnant women, that country would not be doing good. This is the rationale of considering maternal mortality as a public health priority in any country. Sri Lanka reduced maternal mortality over the years to reach the region’s best. But over the last 10 years we are struggling to further reduce it from 30 deaths per 100,000 live births.
Q. What do you consider as a maternal death and a maternal suicide?
A. Maternal death is a death of a woman while pregnant or within 42 days after delivery due to a pregnancy-related or medical cause. We define a maternal suicide as ‘Death caused by self-directed injurious behaviour with an intent to die as a result of the behaviour in a woman who is pregnant or has recently delivered (one year after termination of pregnancy)’. Accordingly not all maternal suicides are classified as maternal deaths, only deaths due to underlying psychiatric conditions are counted as maternal deaths.
Q. How do you obtain information on maternal suicides in the country?
A. Sri Lanka has a National Maternal Death Surveillance and Response System which includes a notification criteria. All public health midwives and hospitals in the country should inform “deaths of all women of reproductive age (15 - 49 years) during the pregnancy or one year after termination of pregnancy irrespective of the cause of death” to the Family Health Bureau within 24 hours. This includes maternal suicides. All such probable maternal deaths are notified, data collected and reviewed at field, hospital and national levels.
Q. Is suicide a leading cause of maternal deaths in Sri Lanka?
A. Suicide is the 4th leading cause of death for women aged 15–49 years worldwide. In the year 2017, Sri Lanka reported 2,586 suicides. Of this 677 (26%) were female suicides.
In Sri Lanka, the leading causes of maternal deaths include mainly, heart diseases, pneumonia and post-partum haemorrhage (bleeding after delivery). Maternal deaths due to suicides are fluctuating. However, every year a significant number of maternal suicides are reported throughout the country.
Q. You said that most of the maternal deaths are secondary to medical illnesses and a fair number of maternal suicides, every year. Yet the maternal deaths secondary to self-harm have been omitted from published rates of maternal mortality. Do you agree?
A. Yes. As I mentioned initially, not all maternal suicides are true maternal deaths. We take only female suicides due to underlying psychiatric illness during or within 42 days of delivery for maternal mortality calculations. However, recently the World Health Organization has recommended that all female suicides during and 42 days after pregnancy to be considered as maternal deaths. Discussions are underway how to include them in the country’s maternal mortality statistics.
Q. Despite growing attention on the prevalence of perinatal mood disorders, estimated at up to 15% of pregnant and postpartum women in the United States, according to the International Public Health Encyclopoedia, what is the incidence in Sri Lanka?
A. Our surveillance data shows that every year 25 -30 maternal suicides are reported throughout the country. The country reported 448 maternal suicides during the period 2002 – 2018. In the year 2018 alone, there were 38 deaths, and a maternal suicide rate of 11.7 per 100,000 live births.
Q. Any recent national study on this?
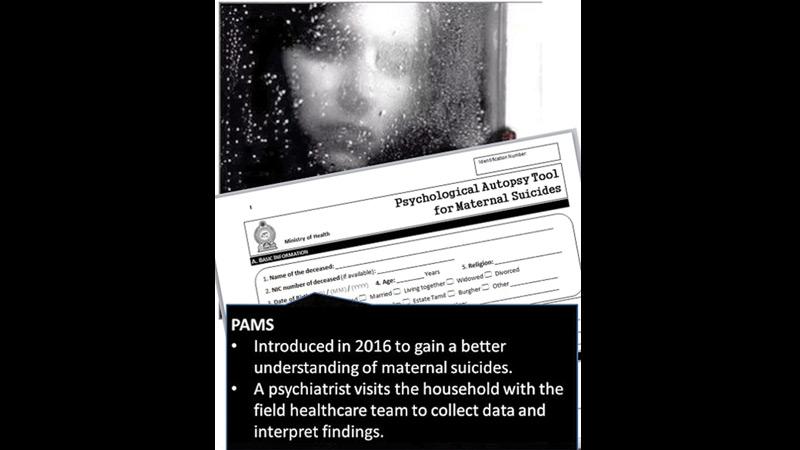
A. We have comprehensive surveillance data reported by field healthcare teams on all maternal suicides. Due to the growing number of suicides in recent years, with the support of the Sri Lanka College of Psychiatrists a Psychological Autopsy tool for Maternal Suicides (PAMS) was introduced to gain better understanding of maternal suicides from the year 2016. A psychiatrist visits the household with the field healthcare team to collect data and interpret findings. Sri Lanka is the only country in the world having such a methodological approach to study maternal suicides.
Q. What are the causes? Do inherited or existing psychiatric diseases in the mother make her more vulnerable?
A. A majority of them are due to sudden impulsive acts arising from complex social scenarios, interpersonal conflicts and lack of family support. A significant proportion (1/3) is also attributed to underlying mental illnesses.
Q. How do these mothers die?
A. Poisoning is the commonest method. Hanging, burning and drowning are other forms of self harm.
Q. Many health experts have cited Post Partum Depression ( PPD) as one of the causes? What is post partum depression?
A. It is a complex disease condition with a mix of physical, emotional, and behavioral changes that happen in a woman after delivery. As its name implies this is a form of major depression originating de-novo within 4 weeks after delivery. It is linked to chemical, social, and psychological changes associated with delivering a baby. Yes, there is a rapid chemical change involving a sharp drop of oestrogen and progesterone hormones within three days after delivery.
Q. What is the most vulnerable period for pregnant women to want to commit suicide?
A. Pregnancy has three trimesters, each marked by specific fetal developments. According to our analysis, primis have more tendency to commit suicide. The majority killed themselves before delivery (antenatal period) and our data shows more suicides in the second trimester. About one third of the maternal suicides are reported in the post-natal period.
Q. Does the age of the mother matter? Is an older mother more vulnerable to suicide?
A. A majority (>75%) were <30 years of age, with a peak in the 26-30 year age group. Sri Lanka data shows that only few older women committed suicide during pregnancy. Many of the victims are married women.
Q..Studies have shown that adolescent girls who have unwanted pregnancies and no coping skills or no advice from parents on how to cope are more likely to resort to self harm. What is the situation in Sri Lanka?
A. When we look at Sri Lankan maternal suicides, this is fairly true. We saw nearly 100 adolescent girls (below 20 years) committing suicide, during a recent study period. Complex psycho-social situations triggered by sudden impulses have ended as maternal suicides. We have identified lack of coping skills as a contributory factor for these deaths. Unwanted pregnancies is a significant contributor (one fourth) of maternal suicides.
Q. Myths? Some believe that pregnancy protects women against these risks. Your comments?
A. The general thinking is that pregnancy lowers the risk of suicide. However, latest literature and studies indicate that pregnant women are at increased risk for suicidal ideation and behaviours compared to the general population.
Q..Do we need more data to address potential social and psychological biases that have led to neglect of the topic of maternal self-harm deaths?
A. Actually, we have rich data. Our surveillance with the Psychological Autopsy Tool is a comprehensive modality to rebuild the story of the deceased woman in different facets. We have also introduced a screening tool to assess the mental health wellbeing of these women and refer them for early psychiatric care.
Q. Based on studies you have done have you made any recommendations that incorporate the whole woman in prenatal care and thus prevention of this devastating outcome?
A. We have done in-depth exploration into these deaths and disseminated to major stakeholders. However, prevention of suicide is complex and difficult. Preventive strategies go beyond health boundaries. The Family Health Bureau is working collaboratively with many agencies to minimize maternal self-harm. We advocate planned pregnancies both physically and mentally. The need for proper contraceptives is crucial. Women should be aware of emergency contraceptives following unprotected sexual encounters to prevent conceiving. We focus on prevention of gender-based violence. We have done a lot in this regard. We introduced the RED Book to capture women in danger of dying due to any factor mainly targeting complex social scenarios, and emphasising the general rules regarding preventing all suicides.
Q.Your message to parents, adolescents and mothers to be on why it is important to avoid self harm during and after pregnancy?
A. Awareness about maternal self-harm by women in reproductive age, is most important to their partners, relatives, caregivers and the general public. Ensuring optimal psycho-social wellbeing of the mothers to be is indispensable in addressing this problem.
