As paediatricians gather this week to share their expertise on breastfeeding amid the Covid- 19 pandemic , the Sunday Observer spoke to an eminent neonatologist at the De Soysa Maternity Hospital, Borella, and Senior Consultant, University of Colombo Neo Natal Unit, Dr Nishani Lucas to find out why breast milk continues to remain as the most nutritious and complete meal for the newborn baby at a time when mothers across the world are increasingly switching to artificial formulae, and in the process, exposing their infants to childhood diseases that hamper their development.
Excerpts …
Q. This is Breastfeeding Week (August 1-7.) Why is a whole week devoted to raising awareness on this very natural act of millions of mothers the world over?
A. The World Breastfeeding Week was first celebrated in 1992 by the World Alliance for Breastfeeding Action (WABA) and is observed in 120 countries by UNICEF and WHO and their partners. WABA was formed in 1991 with the goal to re-establish a global breastfeeding culture and provide support for breastfeeding all over the world.
Q. Global health experts such as the World Health Organization and UNICEF have unanimously declared that breast milk is the best for babies . Do you agree?
 Dr Nishani Lucas |
A. Yes of course, I agree. There is undisputed scientific evidence that breast milk is the best food that can be given to a baby. It increases intellect, improves immunity, promotes jaw growth, reduces allergy, increases bonding and affects early programming reducing non communicable disease in adulthood causing positive effects that last a lifetime.
On the contrary, not giving breast milk or giving any other type of milk will result in negative effects that last a lifetime.
Q.This time Breastfeeding Week is being observed amid fears of the Covid-19 pandemic. Do you think that breastfeeding by a Covid positive mother should be encouraged or discouraged to safeguard the baby? If so why?
A. Breastfeeding should be encouraged in a Covid positive mother. WHO recommends that mothers with suspected or confirmed Covid-19 should be encouraged to initiate and continue breastfeeding with rooming in and uninterrupted skin to skin care. Mothers should be counselled that the benefits of breastfeeding substantially outweigh the potential risks of transmission.
Non breastfeeding the baby increases the mortality risk (10 - 14 times). ).Breast milk of mother with Covid-19 has been found to have protective antibodies (secretory IgA) against Covid-19. (Scientific brief – June 23, 2020 – WHO)
Q.What precautions are in place in our hospitals to protect the infant from being infected while being breastfed by a Covid positive mother?
A. The antibodies produced by the mother against Covid-19 reaches the baby via the mother’s breast milk and acts as a protection for her baby. There is no requirement for the mother to wear gloves.
Hand washing and wearing a mask are the only measures required to minimise the risk of transmission to the baby as per most recent UNICEF guidelines.
Q. In general, at what stage should a normal mother start breastfeeding her newborn baby?
A. A mother should start breastfeeding her baby soon after birth, within the first hour of birth, when the baby indicates that he/she is hungry via the hunger cues with the assistance of the health staff at the center of delivery.
Q. What are the health benefits for the baby if an early start is made to breastfeed her/him?
A. Universally, breastfeeding was ranked the number one intervention of preventing childhood mortality.
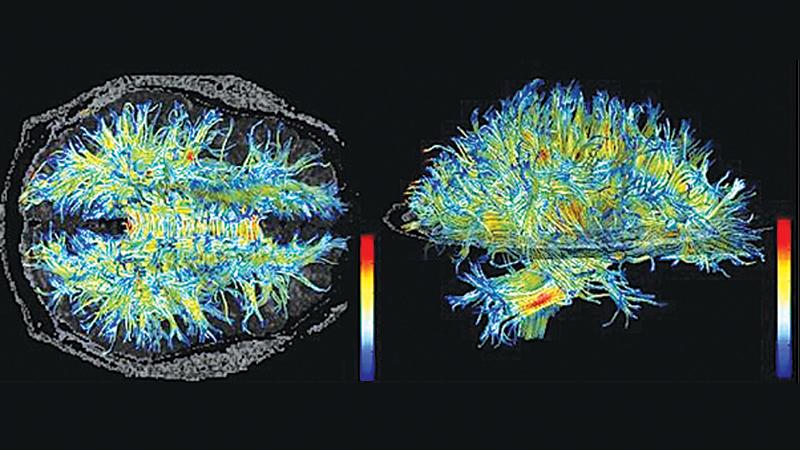
Baby will have a superior intellect with an IQ that is 8-10 points higher with better micro-organisation in white matter of the cerebrum and cerebellum. Breastfed babies have a better immunity due to transfer of multiple immune mediators and a larger thymus.
Baby will also have a markedly decreased risk of respiratory infection (72% less), diarrhoea (64% less), ear infection (50% less), necrotizing enterocolitis (58% decrease) and sudden infant deaths (38% decrease).
Breastfeeding reduces asthma by 9% along with reduction in other allergic conditions. Breastfeeding also develops jaws and airways and reduces malocclusion by 68%.
It also affects early programming with reduction of obesity (26% less), type 1 diabetes (39% less), type 2 diabetes (27% less) as well as hypertension, coronary disease and hypercholesterolaemia. Breastfeeding also reduces the risk of acute lymphoblastic leukemia (1.3 fold) and acute myeloblastic leukemia (1.2 fold), according to studies.
Q. Yet despite awareness raising we see many mothers now switching to bottle feeding at an early stage, some giving up breastfeeding altogether within a short time and introducing their newborn to artificial infant formulae instead, citing various excuses. What are the adverse health impacts of this switch to formulae feeding for the newborn?
A. The baby will miss out on all the benefits that he gets with breastfeeding from newborn to adulthood as mentioned above, along with getting exposed to other harmful effects.
The effect of formula feeding is worse than the harm of tobacco smoking, where smokers of over 20 cigarettes are 3 times more likely to develop lung infection compared to formula fed babies who are 17 times more likely, smokers are twice as likely to have Crohn disease where formula fed babies are 4 times more likely, smokers are 1.5 times more likely to develop asthma compared to formula fed babies who are 1.7 times likely and smoking triples the risk of leukemia where formula feeding increases the risk by 17%.
Formula milk is not sterile and contains harmful bacteria, like Salmonella and Enterobacter sakazakii, which causes neonatal meningitis resulting in 40-80% mortality.
Formula has also been found to contain toxins such as melamine which resulted in renal failure and death in China in 2008, cupric sulphate which is also used as a pesticide and DCD in 2013 in Sri Lanka.
Q. Is it necessary to continue breastfeeding even when you have switched baby to solids?
A. Yes, continued breastfeeding alongside complementary feeding has been ranked as the third most effective intervention to reduce infant mortality. (2003 landmark Lancet Child Survival Series)
Q. Does this mean that breast milk adapts as the baby grows to meet its changing needs?
A. Yes, each mother’s breast milk is tailor-made to suit the requirements of her baby. The composition of breast milk in a mother whose baby is born preterm includes higher protein content and higher immunoglobin content to match the higher requirement of the preterm baby.
Breast milk of a 4-month-old baby will be higher in lactose to match the rising energy requirement and the breast milk of a one-year old infant will be lower in energy content as most energy is provided via the complementary food. However, breast milk continues to supply immunoglobulins, neutrophils and macrophages throughout breastfeeding, protecting the infant from disease.
Q. Do these benefits last a lifetime into adulthood?
A. Yes. Breast milk affects early programming via alteration of epigenetics and the microbiome in a beneficial way where the lifetime risk of obesity, diabetes, hypercholesterolaemia, hypertension, coronary artery disease, multiple sclerosis, inflammatory bowel disease are markedly reduced ensuring that the effects of breastfeeding last a lifetime.
The reverse is of course that even one drop of formula milk increases the lifetime risk of all such diseases.
Q. Apart from the health benefits, it is said breastfeeding promotes closer bonding between mother and child? Why is this bonding important to the newborn baby?
A. The act of breastfeeding not only provides optimum nutrition for the baby but also provides the foundation to form a secure bond with an adult, in this case the mother, during early life, which in turn may become the foundation for forming stable relationships in the future for this newborn baby.
Q. What about the mother? In what sense does this bonding help her mentally?
A. There are studies that have shown that breastfeeding may be protective against mood problems like depression as well as sleep problems in the mother.
Q. Is it also true that breastfeeding boosts a mother’s immunity against certain life threatening diseases?
A. Yes. Breastfeeding reduces the risk of breast cancer by 39%, ovarian cancer by 26% and also endometrial cancer through epigenetics. The mother will also have a decreased risk of anemia as she will have amenorrhea during the period of exclusive breastfeeding.
The hormones mediating breastfeeding will also have a positive effect on the mother’s bone health, as well as act as a contraceptive during the period of exclusive breastfeeding while decreasing mother’s insulin requirement (which is especially beneficial for diabetic mothers).
The oxytocin released during breastfeeding will increase bonding and also reduce the mother’s chances of depression. The calories expended during breastfeeding will also be responsible for weight loss and regaining the prepregnant body shape. Breastfeeding reduces the risk of both diabetes and hypertension in the mother. It also reduces the baby’s risk of developing diabetes and hypertension in adulthood via early programming.
Q. What is your message to all new mothers on the importance of breast milk.
A. Breast milk is a gift that only you can give your child to help him/her enjoy increased intelligence and better health throughout life. Do not deprive your child.
Live up to your parental responsibility. Breastfeeding is not a choice, it’s a duty. Breastfeeding is one of the greatest acts of love that a mother can do for her child. If you are faced with challenges don’t turn to formula milk.
Get skilled support from your local public health midwife or Lactation Management Centres in state hospitals. These are walk in centers, which are dedicated to help babies irrespective of their place of birth.


