Osteoarthritis is on the rise both globally and in Sri Lanka. Unfortunately not many victims of this chronic and common joint condition are even aware they have it until their bones have degenerated to an advanced stage. Caught up in the hectic pace of life, many women often tend to neglect telling signs and symptoms of joint aches and pains which are a warning that all this excessive exercise on their already degenerating joints could have aggravated the onset if not existing wear and tear arthritis commonly known as Osteoarthritis (OA).
 Concerned bone specialists are thus raising awareness on the disease and devoting an entire month for it in order to raise more public awareness on a subject that has been sidelined up to now.
Concerned bone specialists are thus raising awareness on the disease and devoting an entire month for it in order to raise more public awareness on a subject that has been sidelined up to now.
The Sunday Observer asked Head of Rehabilitation Services, MJF Charitable Foundation, Dr. Gopi Kitnasamy who has wide experience in this field to share some of his expertise with our readers.
Excerpts
Q: Osteoarthritis seems to be rapidly increasing among Sri Lankans judging by the number of patients currently undergoing treatment for this condition. Explain what exactly is osteoarthritis?
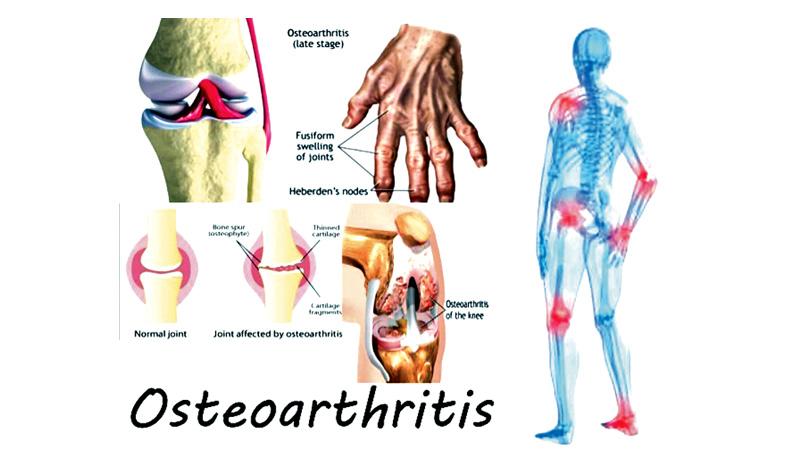
A: Osteoarthritis (OA) is sometimes called degenerative joint disease or ‘wear and tear’ arthritis. It is the most common chronic condition of the joints. It occurs when the cartilage or cushion between joints breaks down leading to pain, stiffness and swelling. In normal joints, a firm, rubbery material called cartilage covers the end of each bone. Cartilage provides a smooth, gliding surface for joint motion and acts as a cushion between the bones. In OA, the cartilage breaks down, causing pain, swelling and problems moving the joint. OA can affect any joint, but it occurs most often in knees, hips, lower back and neck, small joints of the fingers and the bases of the thumb and big toe.
Q: Who are those most at risk of getting it?
A: Although OA occurs in people of all ages, osteoarthritis is most common in people older than 50. Common risk factors include increasing age, obesity, previous joint injury, overuse of the joint, weak thigh muscles, and genes. One in two adults will develop symptoms of knee OA during their lives. One in four adults will development symptoms of hip OA by age 65. One in 12 people 60 years or older have hand OA.
Q: What is the most common form of OA?
A: Osteoarthritis of the knee. It occurs mostly in people 50 years and older, but may occur in younger people, too.
Q: What causes this condition? How long does it take to develop?
A: In OA Knee, the cartilage in the knee joint gradually wears away. As the cartilage wears away, it becomes frayed and rough, and the protective space between the bones decreases. This can result in bone rubbing on bone, and produce painful bone spurs. Osteoarthritis develops slowly and the pain it causes worsens over time.
Q: Symptoms?
A: A knee joint affected by arthritis may be painful and inflamed. Generally, the pain develops gradually over time, although sudden onset is also possible. Other symptoms include:
The joint may become stiff and swollen, making it difficult to bend and straighten the knee.
Pain and swelling may be worse in the morning or after sitting or resting
Vigorous activity may cause pain to flare up. Loose fragments of cartilage and other tissue can interfere with the smooth motion of joints. The knee may ‘lock’ or “stick” during movement. It may creak, click, snap or make a grinding noise (crepitus).
Pain may cause a feeling of weakness or buckling in the knee Many people with arthritis note increased joint pain with rainy or cold weather.
Q: Contributory or risk factors leading to OA?
Age: - Old age is a significant risk factor for development of knee OA, as the joints experience normal wear over time.
Sex: Women are more likely to develop osteoarthritis, though it isn’t clear why
Genes: Various genetic traits can make a person more likely to develop OA. One possibility is a rare defect in the body’s production of collagen, the protein that makes up cartilage. This abnormality can cause osteoarthritis to occur as early as age 20. Other inherited traits may result in slight defects in the way the bones fit together so that cartilage wears away faster than usual.
Weight: Being overweight puts additional pressure on hips and knees. Many years of carrying extra pounds can cause the cartilage that cushions joints to break down faster.
Injury and overuse: Repetitive movements or injuries to joints (such as a fracture, surgery or ligament tears) can lead to osteoarthritis. Some athletes, for example, repeatedly damage joints, tendons and ligaments, which can speed cartilage breakdown.
Bone/joint deformities: Some people are born with malformed joints or defective cartilage, which can increase the risk of osteoarthritis

Certain careers that require standing for long periods of time, repetitive bending, heavy lifting or other movements can also make cartilage wear away more quickly.
An imbalance or weakness of the muscles supporting a joint can also lead to altered movement and eventual cartilage breakdown in joints. Other factors include; bone and joint disorders like rheumatoid arthritis, certain metabolic disorders such as hemochromatosis, which causes the body to absorb too much iron, or acromegaly, which causes the body to make too much growth hormone.
Q: How is it diagnosed?
A: Diagnostic methods include:
Physical Examination where the doctor will examine the joints and test their range of motion (how well each joint moves through its full range). He will be looking for areas that are tender, painful or swollen as well as signs of joint damage. The doctor will examine the position and alignment of the neck and spine. A diagnosis of osteoarthritis may be suspected after a medical history and physical examination is done.
X-rays can show damage and other changes related to osteoarthritis to confirm the diagnosis.
Magnetic resonance imaging (MRI) offers better images of cartilage and other structures to detect early abnormalities typical of osteoarthritis.
Q: Is it curable? Treatable? If so how?
A: There is no cure for arthritis, but there are a number of treatments that may help relieve the pain and disability it can cause. Initial treatment is nonsurgical. Your doctor may recommend a range of treatment options. They include: Lifestyle modifications in your daily life, which can protect your knee joint and slow the progress of arthritis; minimising activities that aggravate the condition, such as climbing stairs. Switching from high impact activities (like jogging or tennis) to lower impact activities (like swimming or cycling) will put less stress on your knee. Losing weight can reduce stress on the knee joint, resulting in less pain and increased function.
Q: As a Physiotherapist, how does Physiotherapy help OA patients?
A: Our treatment includes both Exercise and Electrotherapy like SWD, Ultrasound, and Laser, with specific exercises to increase range of motion and flexibility and strengthen the muscles in your leg. Your Physiotherapist will develop an individualised exercise program that meets your needs and lifestyle.
Q: Are there any other options?
A: Use of assisted aids such as a cane, wearing shock-absorbing shoes or inserts, or wearing a brace or knee sleeve can be helpful. A brace assists stability and function and may be especially helpful if the arthritis is centered on one side of the knee. These should be used only for a short period as using braces and support for long periods can weaken your muscles supporting the knee.
Q: Other remedies?
A: Applying heat or ice, using pain-relieving ointments or creams, wearing elastic bandages to provide support to the knee may provide some relief from pain. Alternative therapies to treat pain include the use of acupuncture and magnetic pulse therapy. If you do try them, find a qualified practitioner and keep your doctor informed of your decision.
Q: What about medications?
A: Several types of drugs are useful in treating arthritis of the knee. Because people respond differently to medications, your doctor will work closely with you to determine the medications and dosages that are safe and effective for you.
Q: What about surgery? When is it recommended?
A: Your doctor may recommend surgery if your pain from arthritis causes disability and is not relieved with non-surgical treatment. Rehabilitation post-surgery must be properly supervised which is very important for the full recovery and returning back to normal.
Q: Can eating the right food prevent arthritis?
A: A diet rich in fruits and vegetables has been shown to help reduce inflammation and pain in your joints. Antioxidants may help prevent arthritis, slow its progression, and relieve pain. Being at a healthy weight is a critical component to managing OA of the knees. The antioxidant vitamin C is necessary for cartilage development. A lack of vitamin C can lead to weakened cartilage and increase osteoarthritis symptoms. Some research shows that vitamin D can help prevent the breakdown of cartilage, and decrease the risk of joint space narrowing. The healthiest fats for people with osteoarthritis (or other inflammatory disorders) are omega-3 fatty acids. Some foods which are rich in omega-3 are salmon, herring, mackerel, sardines, anchovies, rainbow trout, Pacific oysters, omega-3-fortified eggs, flaxseed and walnuts. Some spices have anti-inflammatory effects, too. Among the most promising are ginger and turmeric.
Q: Exercise?
A: Exercise is the best non drug therapy for OA.
The best exercises are strengthening exercises to maintain and improve muscle strength. Strong muscles can support and protect joints that are affected by arthritis. Two types of exercise are particularly good for most people with osteoarthritis. Walking lowers the risk of fractures (by stopping or slowing down the loss of bone mass) and tones muscles that support joints, but avoid going for long walks and walking on hills.
Aquatic (in water) exercises, particularly helpful for people just beginning to exercise as well as those who are overweight. Aquatic exercises do not involve swimming; rather they are performed while standing in about shoulder-height water. The water helps relieve the pressure of your body’s weight on the affected joints (hips and knees in particular), while providing resistance for your muscles to get stronger. Regular aquatic exercise can help relieve pain and improve daily function in people with hip and knee OA.
Q: Will water exercise help those with obesity problems since obesity is one cause for OA?
A: Overweight and obese adults may have functional limitations that result in difficulty performing traditional weight-bearing exercises and activities. Water exercise is a commonly recommended alternative due to the potential therapeutic qualities of water. Weight loss involves burning more calories than a person ingests. Understanding this one basic fact takes the magic and intimidation factor out of the weight-loss equation. Water exercise allows people to work out longer at lower intensities, thereby burning more calories than shorter duration, high-intensity exercise.
Q: Your advice to patients?
A: Lose weight, eat right and exercise. Avoid wearing pointed and high heels. Use appropriate footwear.
