The resurgence of Covid-19 in some countries including Sri Lanka, and the seasonal influenza virus circulating across the world has led to a surge in respiratory infections, prompting the chest physicians to urge those susceptible to developing respiratory infections to take precautions against them without delay.
Here, Consultant Respiratory Physician, District General Hospital and District Chest Clinic Trincomalee, Dr. Upul Pathirana explains what causes many of these infections, how to treat them and most importantly how to avoid them with easy to follow simple hygienic measures.
Excerpts
 Q: Pulmonary infections such as pneumonia are now on the rise across the world. Of these infections what are the most serious diseases associated with pulmonary infection that you find in Sri Lanka and what part of the body is affected by them?
Q: Pulmonary infections such as pneumonia are now on the rise across the world. Of these infections what are the most serious diseases associated with pulmonary infection that you find in Sri Lanka and what part of the body is affected by them?
A. The infections hit on the respiratory system starting from nose to lungs and pleura. The medical community names these infections based on the anatomical sites and involved organisms. Covid-19 pneumonia is one of our concerns since December 2019 and there is a resurgence of Covid-19 in some countries including Sri Lanka. Seasonal influenza virus is circulating all over the world and it is one of the concerns for us as well.
Q: Can anyone get respiratory infections?
A. There are people who are susceptible to develop respiratory infections even though any of us can catch such infections. Individuals with risk factors are prone to develop severe infections and complications; otherwise it might be an acute simple self-limiting disease in most of the healthy persons.
 Q: As Pneumonia is one of the most critical and common of these infections what exactly is pneumonia?
Q: As Pneumonia is one of the most critical and common of these infections what exactly is pneumonia?
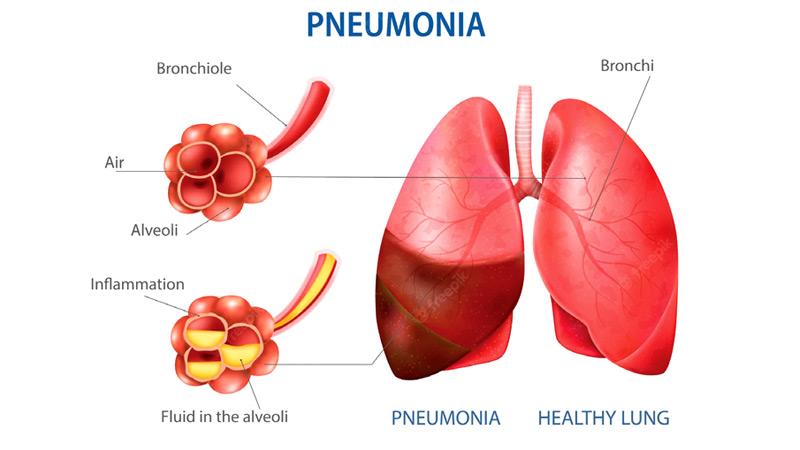
A. There is a spectrum of bugs including viruses, bacteria, fungi and parasites, which can cause respiratory infections. We call it pneumonia when affecting the air sacs (alveoli) within the lungs. Uncomplicated infections such as rhinitis and pharyngitis (affecting the nose and pharynx respectively) are more common than pneumonia.
Q: Are there different types of pneumonia? If so, name the most common in this part of the world?
A. We classify pneumonia based on the site involved within the lungs, causative factor, involved organism, acquired environment and many more. Microorganisms might not be the source of pneumonia in some instances but it might be following recurrent and long-standing exposure to some environmental particles at your home or working environment. Rarely, our own immune system stands against body tissues and gives rise to pneumonia, which needs specific treatment guided by a respiratory physician. Either bacteria or viruses cause by far the commonest pneumonia and it is acquired from the community in most cases.
Q: Is it contagious? How?
A. Even though the human-to-human transmission is well recognised in pneumonia, there is no evidence to say that this is true for all types of pneumonia. Most of the viral pneumonias spread rapidly within the community through air, droplets and/or contact routes. Pulmonary tuberculosis is one form of pneumonia with distinct features and it passes on to others from an infected person who has active disease.
Q: If air-borne what is the distance that the virus travels if one is in the same room when he or she coughs or sneezes?
A. This is a bit complex and technical topic and I will simplify for better absorption. The respiratory infections are transmitted through particles of different sizes. The particles could be either more than or less than 5 μm and they are called respiratory droplets and droplet nuclei respectively.
 Droplet transmission occurs when a person is in in close contact (within 1 m) with someone who has respiratory symptoms (e.g., coughing or sneezing) and is therefore at risk of having his/her mucosa (mouth and nose) or conjunctiva (eyes) exposed to potentially infective respiratory droplets.
Droplet transmission occurs when a person is in in close contact (within 1 m) with someone who has respiratory symptoms (e.g., coughing or sneezing) and is therefore at risk of having his/her mucosa (mouth and nose) or conjunctiva (eyes) exposed to potentially infective respiratory droplets.
Airborne transmission is different from droplet transmission as it refers to the presence of microbes within droplet nuclei, which can remain in the air for long periods of time and be transmitted to others over distances greater than 1 m.
Q: What precautions should one take to prevent getting infected?
A. The source control is one of the best strategies to minimie or prevent respiratory infections. Practicing hand hygiene is a simple yet effective way to prevent infections. A person with symptomatic illness has the potential to infect others even though an infected asymptomatic individual also spreads the disease. Therefore, if you have flu-like symptoms or any other respiratory symptoms, wear a facemask to cover your mouth and nose. The Centres for Disease Control and Prevention (CDC) also recommend sneezing into a disposable tissue, and then throwing it away and washing your hands clean. However, if you can’t access a tissue in time, sneezing into your elbow is the next best option to sneezing into the air.
Q: Can you give us a simple demonstration of these rules?
A. l Bury your mouth and nose in your inner elbow.
lSneeze, and then wait a few seconds to see if there is another sneeze on the way.
lIf you touch your sleeve, wash your hands before touching anyone or anything.
Q: Are respiratory infections curable?
A. The vast majority of respiratory infections are self-limiting or settle with symptomatic treatment as they are viral in origin. However, for pneumonia regardless of viruses or bacteria, you should seek medical advice early as timely intervention can cure pneumonia in most cases.
Q: Is it fatal especially if it affects the lungs?
A. Yes. Pneumonia is one of the most serious infections that affect humans. One suffering from pneumonia may develop complications like respiratory failure or septic shock (a state of low blood pressure) necessitating Intensive Care Unit (ICU) treatment. Mortality is high in severe complicated pneumonia all over the world.
Q: How do you prevent it?
A. Respiratory hygienic measures such as good hand hygiene, protective facemask, and avoiding sneezing or coughing in crowded places minimise the spread of infection. BCG vaccine administered to all newborns prevents complications of Tuberculosis in early childhood. Influenza and Pneumococcal vaccines can prevent influenza and pneumococcal pneumonia. There are many more to discuss about preventive measures and it is beyond the scope of this article.
Q: Who are those most at risk of getting it? Why?
A. Any of us can catch respiratory infections although individuals with risk factors are prone to develop more severe infections and complications. Uncontrolled blood sugar is one of the commonest reasons to acquire any type of severe infections including pneumonia. Less ambulatory people, patients with neurological disorders and other organ failures, cancer patients, chronic lung disease, people living with Acquired Immunodeficiency Syndrome (AIDS), malnutrition and those on medications which impair the immune system are at most risk.
Q: What about persons with underlying lung diseases including cystic fibrosis, asthma, or chronic obstructive pulmonary disease (emphysema)?
A. The patients with chronic lung diseases are at risk of acute exacerbations of their underlying lung disease due to respiratory infections.
Q: Those who have had a recent viral upper respiratory tract infection including influenza- are they too vulnerable?
A. Yes, although these infections look very simple, they can damage the surface of the wind tubes (airway epithelium) favoring adhesions and establishment of secondary bacterial infections.
Q: What are the symptoms to look out for?
A. Runny nose, sneezing, nasal block, sore throat, painful swallowing, cough and fever are the commonest of upper respiratory tract infections. When the organisms reach the lungs causing pneumonia, the patients develop high swinging fever, productive cough with yellow or rusty sputum, reduced appetite, chest pain during breathing and breathlessness. Extremes of ages such as elderly people can have unusual presentations like confusion as the sole manifestation of pneumonia.
Q: Who should patients with any of these symptoms consult initially?
A. A consultation with your family doctor is enough in most cases. However, if you are sicker, you can straight away seek institutional care from a hospital. Those with risk factors should consult a doctor as early as possible.
Q: How is it detected?
A. The doctors make the initial diagnosis after listening to the patient and carrying out physical examination. Initial blood investigations, sputum testing and chest x-ray in selected cases will confirm the diagnosis.
Q: Who makes the final diagnosis? What is the procedure involved?
A. After assessing the patient, the doctor will direct you for either home based care or institutional care. An experienced physician attends to all the pneumonia patients and decides the level of care such as in-ward or Intensive Care Unit.
Q: What tests are required for the patients to undergo? Why are they necessary?
A. The objectives of testing are to first confirm the pneumonia and then identify the causative organism. These patients might undergo further investigations to catch complications and to monitor the disease course and treatment. The investigations include sputum testing, blood investigations, imaging like X-ray, ultrasound and Computed Tomography. In selected cases, fibro optic bronchoscopic examination and sampling will be helpful.
Q: What are the complications (short term and long term) of Pneumonia?
A. Pneumonia affects your lungs through which the oxygen from the environment is entering your blood. Therefore, the oxygenation can be failed when the pneumonia is severe and it is called respiratory failure. Due to the effect of toxins produced by the involved microorganisms and our own body’s reaction to infection could create a state of low blood pressure called septic shock. There are other complications like lung abscess and pleural effusion (fluid between lung and chest wall). Despite the fact that even severe pneumonia can recover completely without any long-term consequences, some patients can have persistent residual lung damage.
Q: How do you treat pneumonia?
A. The mainstay of treatment is antibiotic and antiviral therapies. They need other supportive care for overall management.
Q: Is the treatment given tailored to the needs of the patient? Or is it a blanket treatment for all?
A. One size fit for all theory has now moved away from the medical practice. All the treatments are individualised in pneumonia patients as directed by an experienced physician.
Q: What is the usual recovery period?
A. There is no black and white answer in the form of number of days for recovery period. The recovery is quick within a few days in some cases and others it is prolonged.
Q: Do you have a message for our readers on avoiding risks of pneumonia? Any Do’s and Don’ts they should follow?
A. Good respiratory hygiene will protect you and those around you. If you are infected with a respiratory infection, act responsibly to prevent transmission of infection to others. Be alert and if there are alarming symptoms such as breathlessness consult a doctor early. Regular treatment under the supervision of your family doctor or relevant specialty doctor for those who have chronic diseases can reduce the morbidity and mortality associated with respiratory infections. Diabetes is a common disease in our country and those with uncontrolled blood sugar are at risk of complications including severe respiratory infections. Therefore, you should make sure that you periodically check blood sugar and keep it well controlled.
