In a few days specialists involved in dealing with Hansen’s disease (Leprosy) will come together to discuss ways and pool resources on how to give patients suffering from this disease a better quality of life and most importantly how to detect signs of the disease early so as to prevent it from progressing.
Considered one of the oldest infectious diseases in the world including Sri Lanka, new interventions by Leprosy specialists has led to a drastic decline in the disease until recently the Epidemiology Unit in Sri Lanka reported a sudden surge in the disease both among adults and children , but mainly among children especially in the Batticaloa district.
To aggravate matters, rumours and myths swirling around the disease have left the public at large confused as to what action they should take if a family member showed symptoms of the disease.
The Sunday Observer sought the help of Consultant Dermatologist, Anti Leprosy Campaign, Dr. Indira Kahawita to find out more about this disease, how to detect and prevent it while debunking the myths and prejudices around it to overcome obstacles preventing optimal care to patients .
Excerpts
 Q: Although leprosy is an ancient disease in Sri Lanka and the world, many people are still ignorant of what the disease is , how it is caused and what its symptoms are. . What is Leprosy? How does it spread?. What part of the body does it affect?
Q: Although leprosy is an ancient disease in Sri Lanka and the world, many people are still ignorant of what the disease is , how it is caused and what its symptoms are. . What is Leprosy? How does it spread?. What part of the body does it affect?
A. Leprosy is a chronic infection of the skin and peripheral nerves due to a bacterium, Mycobacterium leprae. It is spread by droplets from an infectious patient’s nose and mouth getting into the respiratory tract of a healthy person. Prolonged contact over a period of several months is necessary for transmission. Only a minority (10 percent) of those infected will manifest symptoms. The incubation period can be as long as 5-6 years. Leprosy is not spread by touch.
Q: Are there different types of Leprosy?
A. There are two varieties, the non infectious or paucibacillary and infectious or multibacillary variety. Those who have less than 5 skin lesions belong to the noninfectious category while those with many skin lesions, nerve involvement and presence of bacteria in the skin belong to the infectious variety.
Q: Can one inherit leprosy?
A. No, it is not a hereditary illness.
Q: Can leprosy be passed from mother to child, or sister to brother via one’s genes?
A. No. the bacterium does not cross the placenta or is not passed through genes. But more than one person in a family can be affected as they are under the same living conditions where prolonged exposure is likely to occur.
Q: Signs of leprosy?
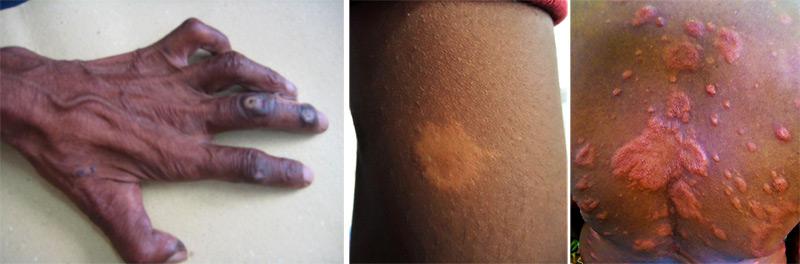
A. The commonest symptom of leprosy is a dry patch of skin which is light coloured and has impaired or loss of sensation within. Usually there are only a few patches, occurring in the face, trunk or limbs. When the disease spreads the number of lesions increases and the patches may become raised from the surface. When there are numerous skin lesions they may show normal sensation within them. Early nerve damage may present as inability to perform fine tasks using fingers or numbness over the hands or feet.
If left untreated they may end up with severe nerve damage leading to deformities. Such nerve damage may also lead to ulcers in the palms or soles. When the bacterium spreads over the whole body, patients may develop changes in the appearance of the face. The facial skin thickens with loss of eyebrows and appearance of nodularity over the forehead. Nodules appear over the earlobes and the chin and lip. Nasal stuffiness and change in voice may also occur. It is such patients who harbor many bacteria in their mucosal surfaces and can spread the disease to others. By this time they do have severe numbness of hands and feet with chronic non healing ulcers.
 Q: Can anyone get leprosy? What about children and infants?’
Q: Can anyone get leprosy? What about children and infants?’
A. Yes, anyone can get leprosy, including children though it is rare in infancy.
Q: Recently the Anti Leprosy Campaign at the Health Ministry was quoted stating there was a sharp spike in leprosy cases in Sri Lanka and that the Western Province and the districts of Anuradhapura and Kurunegala have been identified as Leprosy high risk zones in terms of transmission. Your comments?
A. There is no true spike, but there was less detection of cases during 2020 and 21 due to the pandemic and the resultant adverse conditions in the country. The high numbers we have seen during the past few months are the patients who had the disease but were not detected earlier. Most of the cases in Batticaloa were due to active case finding activities by the public health authorities.
Q: The Campaign spokesperson was also reported as saying that an alarming rate in the spread of the disease was found among school children – with around 15 percent of the cases reported this year being among schoolchildren. How did this happen especially since until recently the majority of cases were detected mostly in older people- well past their teens?
A. For the past 20 years Sri Lanka has reported a child rate (percentage of children below 15 years) of around 10 percent. The current global figure is around 4 – 7 percent. This means that Sri Lanka has a high child rate. Occurrence of leprosy among children indicates that the disease is still being transmitted actively within the country. The very high child rate in 2022 was mostly due to a large number of children being detected during active case finding activities, especially in the Batticaloa district. In my opinion we need to detect cases early, in both children and adults, to interrupt the chain of transmission. In addition each child case has to be investigated with special emphasis on examining the family members to look for other persons with leprosy. A study done among children showed that in about 30 percent of them at least one other family member is affected.
Q: Treatment- How do you treat them? Is it the same for infants, the young and the older victims?
A. There is an effective treatment called Multi Drug Therapy (MDT) consisting of 2 or 3 drugs given over 6 or 12 months depending on the severity of the disease.
The same drugs are given at different dosages to children. The treatment comes as blister packs, provided free of charge by the World Health Organisation (WHO).In addition other drugs may be used to treat nerve damage when necessary.
Q: Is there a vaccine to prevent leprosy?
A. No vaccine is currently available for mass use. Some vaccines are at the stage of testing among test populations. We are hopeful that they will be available for use in the near future.
Q: Diagnosing Leprosy- Who does this? Can any health worker be able to do it?
A. Any health worker should be able to suspect leprosy. The confirmation of the diagnosis and treatment is done under the care of a Consultant Dermatologist in skin clinics throughout the country.
Q: When a person with suspicious signs comes to a clinic what is the usual procedure you follow?
A. The diagnosis is confirmed, either on clinical criteria or with the aid of investigations. There is no blood test to confirm leprosy. Sometimes we use tests on the skin like smears and biopsies to confirm.
Once the diagnosis is confirmed patients are started on MDT according to their age and severity of symptoms. They have to undergo routine blood tests during treatment to ensure that side effects do not occur. Each case is notified to the public health authorities to ensure examination of household contacts and continuation of treatment without interruption. We take special precautions to ensure the privacy of the patients during public health activities.
Q: Can Leprosy be cured if detected early?
A. Yes. Early detection and treatment is paramount in preventing permanent nerve damage.
Q: Once treated and cured can a patient get re –infected?
A. Reinfection is very rare, occurring in about 1%.
Q: When is someone considered non-infectious to others after starting treatment?
A. A patient is considered noninfectious within a week of starting treatment.
Q: What happens to a victim if the condition is untreated for some reason?
A. if a patient with early symptoms remains untreated the bacterium can spread all over the body, leading to more pronounced changes in the skin. Early nerve damage can be treated successfully, but if it goes on for long the damage can be permanent.
This is how people end up with severe deformity due to leprosy. In addition they can transmit the disease to others.
Q: The main obstacles that prevent patients from seeking early treatment?
A. Lack of awareness about the disease and the reluctance to seek treatment as early lesions do not cause much symptoms are the main obstacles.
Q: What are the most common myths about Leprosy in Sri Lanka ?
A. Leprosy is not hereditary, contrary to popular belief. It can occur in the same household like any other infectious disease. Leprosy does not lead to “falling off of fingers”. But fingers can get shortened due to ulceration in severe nerve damage.
Q: How has the Anti Leprosy Campaign met this challenge?
A. Anti Leprosy Campaign has started an islandwide awareness programme to promote patients to seek treatment. Special programs are carried out to detect leprosy among children and household contacts of diagnosed patients. Health staff is trained to detect cases. We operate a Facebook page and YouTube channel “LIFE Sri Lanka” which contains a wealth of information about the disease.
Q: hat is the theme for this year’s Leprosy Day? How meaningful is it to Lankan leprosy patients?
A. This year’s theme is, “Act now. End leprosy” This is extremely relevant to us and we are doing our best to get the whole country on board.
Q: What will be your main focus?
A. Focus is on detecting and treating children with leprosy to interrupt the transmission.
Q: In our technologically advancing nation how do you see the future for leprosy patients in Sri Lanka?
A. We are hopeful that new diagnostic tests and a vaccine will be available in the near future. Testing of new treatments is also happening in other countries.
Q: Gaps you’d like to fill in ensuring optimum benefits in care for leprosy patients?
A. The main gap is in awareness. We would like each Sri Lankan to be aware that leprosy is still among us.
Q: Your message to the general public?
A. Leprosy is still among the Sri Lankan public. Early detection and treatment can lead to complete cure. Leprosy is not a disease to be feared or a reason for discrimination or stigmatisation. A patient on treatments for leprosy can lead a normal life among others.
Q: Your message to persons with suspected symptoms reluctant to seek treatment?
A. Please come for treatment. This will ensure you a disability free life as nerve damage needs prompt treatment.- besides not spreading the disease among others.
