Epilepsy is a common neurological condition globally and in Sri Lanka. Unfortunately, despite effective treatment available to them many Sri Lankans delay seeking treatment early due to myths surrounding this condition.The Sunday Observer asked the President of the Epilepsy Association of Sri Lanka (EASL) Dr. Kishara Gooneratne to spell out some of the main causes for Epilepsy and emerging risk factors that currently put vulnerable persons including schoolchildren at risk to the development of this common neurological condition.
Excerpts.
Q. On February 14 neurologists from across the world will pool their resources and knowledge to discuss Epilepsy- a troubling health issue which still eludes proper understanding. So tell us, what exactly is Epilepsy?
A: Epilepsy affects the brain and causes frequent seizures. Seizures are bursts of electrical activity in the brain that temporarily affect how it works.
Q. Are there different types of Epilepsy? If so, which of them are the most common types in Sri Lanka?
 Dr. Kishara Gooneratne |
A: There are four types of epilepsy which are defined by the type of seizure a person experiences. They are: 1) generalised epilepsy, 2)focal epilepsy, 3) combined generalised and focal epilepsy and 4)unknown epilepsy. People with generalised epilepsy experience seizures that affect both the left and right sides of the brain. In patients with focal epilepsy seizures only affect one part of the brain. In combined generalised and focal epilepsy seizures are of both types mentioned previously. If seizures cannot be determined to be either generalised or focal then patients have an unknown epilepsy. Focal epilepsies are more common than generalised epilepsies both in children and in adults and are thought to be the same in Sri Lanka. It is estimated that approximately 200,000 Lankans have epilepsy
Q. Which is most severe? Why?
A: Developmental and Epileptic Encephalopathy refers to a group of severe epilepsies that are characterised both by seizures, which are often drug-resistant, as well as encephalopathy, which is a term used to describe significant developmental delay or even loss of developmental skills especially affecting children. Seizures in such epilepsies can be focal, generalised or a combination of both.
Q. Can these seizures cause brain damage ? If so, how ? Which part of the brain is harmed?
A: Yes to the first question - prolonged seizures can cause brain damage. However, the length of time seizures need to continue to cause such damage depends on the type of seizure. For example, for generalised tonic-clonic seizures in which the body goes stiff and subsequently shakes, the period that can result in permanent damage to the brain is 30 minutes. The condition in which seizures are prolonged causing such damage is called Status Epilepticus. Uncontrolled epilepsy with a high seizure burden can also permanently alter brain architecture. Lack of oxygen and the biochemical cascade that occurs in nerve cells (neurons) result in this change and damage. Often the location of maximum damage is dependent on where in the brain the seizures originated from.
Q. Is the damage to the brain reversible? What is the time duration for a seizure usually?
A: Often not. However, such damage is not caused by the majority of seizures which last less than 2 minutes..
Q. If a close relative has epilepsy what are the chances of a person in the same family inheriting it?
A: If this is a genetic epilepsy the chance of inheritance depends on the nature of the genetic defect and can range from 5 percent to as high as 50 percent.
Q. What are the risk factors for these brain attacks?
A: There are causes rather than risk factors for the development of epilepsy. They include: genetic, infectious, inflammatory, metabolic and structural and differ for each person. Infection is probably the most common cause of epilepsy worldwide. If there is proof of a brain infection that leads to seizures, this is considered an infectious cause of epilepsy.
Some examples include cerebral malaria, meningitis, viral encephalitis. and congenital infections. There are also certain abnormal structures in the brain that can increase the risk of seizures. This might be something one is born with or developed later in life. Most structural causes can be seen on imaging of the brain with an MRI.
Q. So at what stage is someone most vulnerable to developing seizures and subsequent epilepsy?
A: During the perinatal period (just before and after birth) when the developing brain is most at risk especially from causes such as lack of oxygen to the brain of the fetus or newborn.
Q. Recent media reports revealed that some schoolchildren at pre- puberty age are now taking harmful drugs including Ice. Can drug abuse lead to a brain seizure?
A: Yes, many recreational drugs, especially stimulants such as cocaine, ‘crack’, angel dust (PCP), ecstasy and speed (amphetamines), have the potential to cause seizures. Having prolonged drug-induced seizures and prolonged drug abuse can lead to permanent chemical changes in the brain that can then develop into epilepsy.
Q. What about alcohol?
A: Seizures related to alcohol abuse are encountered more commonly than with any other form of substance abuse. It is also a trigger for seizures in patients with pre-existing epilepsy.
Q. Does stress bring on an attack?
A: Stress is not a cause for epilepsy. Stress, anxiety and depression can trigger seizures in people suffering from epilepsy. Concurrent anxiety and depression are commonly seen in certain types of epilepsy especially focal epilepsy in which seizures originate from a place in the brain called the temporal lobe.
Q. Once a person gets an epileptic fit can he /she get another seizure again?
A. If one experiences a seizure for the first time the likelihood of another occurring depends on certain factors, For example, if a structural lesion is present on brain imaging there is increased risk for subsequent seizures to occur making such a person an epileptic.
Certain types of focal epilepsies can have seizures occurring in clusters. For example, epilepsy involving the part of the brain called the frontal lobe tends to cluster and if one experiences a seizure, one is likely to experience further seizures in succession.
Q. How do you usually detect a potential epileptic patient brought to a clinic?
A: By obtaining information of the events experienced by the person attending the clinic. Doctors will interview the patient and try to obtain eyewitness accounts of the episode or episodes experienced by the patient to make an accurate diagnosis of epilepsy. They will order further tests such as brain imaging and electro-encephalogram to further clarify the type of epilepsy.
Q. As we are in a hi tech era has Sri Lanka access to any new methods to detect early signs of brain attack developing in a person?
A: Unfortunately no. It is when a seizure occurs that we are able to diagnose epilepsy.
Q. Treatment wise – how is epilepsy treated and by whom? What are the methods used?
A: When a patient is diagnosed with epilepsy we (paediatric and adult neurologists, physicians, paediatricians) often initiate an anti-seizure medication which is appropriate to the type of epilepsy.
Treatment includes medicines called anti-seizure medication. Such medication can be effective in 70% of patients. However, in the rest who do not respond, other treatment options such surgery to remove part of the brain responsible for epilepsy, implanted electrical devices that produce electrical pulses which are transmitted to parts of the brain and special diets such as the ketogenic diet can be used.
Q. Does Epilepsy always need to be treated in a hospital ? Can a person who gets an epileptic fit suddenly be treated at home/office ?
A: Not every seizure experienced by patients with epilepsy needs to be treated in a hospital. This is because most seizures self-terminate within 2 minutes and do not cause permanent brain damage. However, if the seizure is prolonged then it would be advisable that such seizures are treated in a hospital setting, as such seizures can result in permanent brain damage and even death.
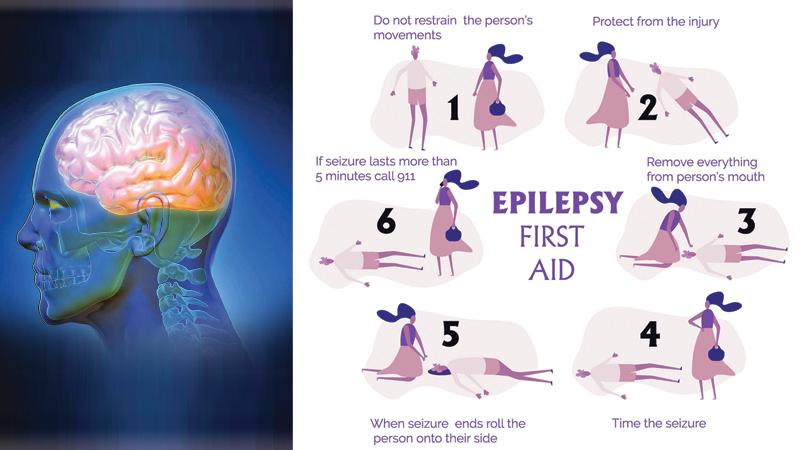
Q. Do you have some simple guidelines as to how to deal with a patient who gets an attack at home till the ambulance arrives?
A: The following are things one can do to help someone who is having a generalised tonic-clonic seizure at home:
1. Ease the person to the floor.
2. Turn the person gently onto one side. This will help the person to breathe.
3. Clear the area around the person of anything hard or sharp. This can prevent injury.
4. Put something soft and flat, like a folded shirt, under his or her head as a cushion.
5. Remove eyeglasses if the person is wearing them.
6. Loosen ties or anything around the neck that may make it hard to breathe.
7. Time the seizure. Call 119 if the seizure lasts longer than 5 minutes.
Q. The theme for International Epilepsy Day 2023 will focus on the stigma people living with epilepsy face around the world. How relevant is it for Sri Lankan Lankan epileptics especially?
A: The theme chosen, which will focus on the stigma people living with epilepsy face around the world, is especially relevant to Sri Lanka, where myths and misconceptions as well as stigma relating to epilepsy are rampant within our society.
This has adversely affected the education, employment, marriage, and social functioning of individuals afflicted with epilepsy. The main goal for International Epilepsy Day 2023 is thus to dispel such misconceptions and social stigma.
Q. Could you cite some examples of common misconceptions relating to Epilepsy?
A: The belief that Epilepsy is a disease caused by gods or a manifestation of the supernatural is still held firmly among segments of the community resulting in people resorting to very primitive forms of treatment such as “exorcisms”. This leads to a delay in treatment despite available resources.
Q. How would you like to see these gaps filled?
A: A greater concerted effort by the government, Health Ministry, health institutions, media, professional organisations/associations and individual professionals in educating the public on epilepsy will quell such misconceptions. Social media is a powerful medium in which peoples’ ideas could be moulded and thus could be an effective conduit to reach out to the community with regards to stigmatisation in epilepsy.
Q. Intervention - wise what has the Epilepsy Association of Sri Lanka ( EASL) of which you are President done in the past few years to create a safer world for Epileptics in this country?
A: Over the years, EASL has tried to quell the misconceptions and stigma associated with this disorder through various public awareness programmes using different media.
Members of the EASL (who mainly comprise medical professionals who treat patients with epilepsy, carers of patients with epilepsy and indeed patients themselves) use print media, electronic media such as television and radio, and social media to reach out to the community and spread awareness of this disease.
Q. Your message to those caring for Epilepsy patients and those afflicted by it?
A: To parents and guardians I wish to reiterate that Epilepsy is a disorder of the brain and effective treatment is readily accessible through our healthcare services.
To those with Epilepsy my message is that with effective treatment you can lead a normal and healthy life, get married, and enjoy opportunities available for education and employment like everyone else.
