Tharindi Wijesiriwardena, (25) from Pannipitiya took her own life due to an emotional breakdown on June 3. Her decision has caused immense distress to her family and friends.
The Sunday Observer spoke to the chief engine driver of the Colombo-Badulla Podimenike express train D.S. Kumarasinghe. “About 9.30 am on June 3, I saw a girl coming towards the railway line in Peradeniya. As the train came nearer, she turned towards the Penideniya railway station and bent on the railway line. She was run over by the train.”
According to the Peradeniya Police Chief Inspector, Kamal Ariyawasna, she was a demonstrator attached to the Peradeniya University’s Science Faculty and had been awarded the degree at the university’s convocation held on May 25.

This is the latest in a series of suicides that had gained public attention recently. The first ever comprehensive report released by the World Health Organisation (WHO) on suicides has ranked Sri Lanka as having the fourth highest suicide rate in the world out of 172 countries. According to the latest report, the suicide rate in Sri Lanka is 28.8 for every 100,000 people against the global average of 11 per 100,000.
Decline
Nivendra Uduman, Counselling Psychologist at Samutthana - The King’s College London Resource Centre for Trauma, Displacement and Mental Health spoke to the Sunday Observer about suicide in young people and coping mechanisms that one can adopt. He said “Suicide is a global public health concern that carries a significant health, economic and social burden. Sri Lanka had one of the highest suicide rates in the world in 1995 and there has been a decline in the number of reported deaths by suicide since then, but we still see a rise in the number of suicide attempts. This is prevalent in all social strata, in varied contexts and forms.”
“Education as we perceive it in Sri Lanka, has very little to do with whether young people attempt suicide or not. There are factors such as interpersonal dynamics, the presence or absence of coping skills, impulsiveness and mental illness that also play a role in young people attempting to end their lives. ‘Education’ that we receive in school or university in Sri Lanka does not really focus so much on emotional well-being, interpersonal skills, problem solving skills etc as much as it focuses on academics, achievements and success. Hence, young people in both urban and rural settings often do not possess skills to cope with crisis/problems in their lives,” Uduman said.
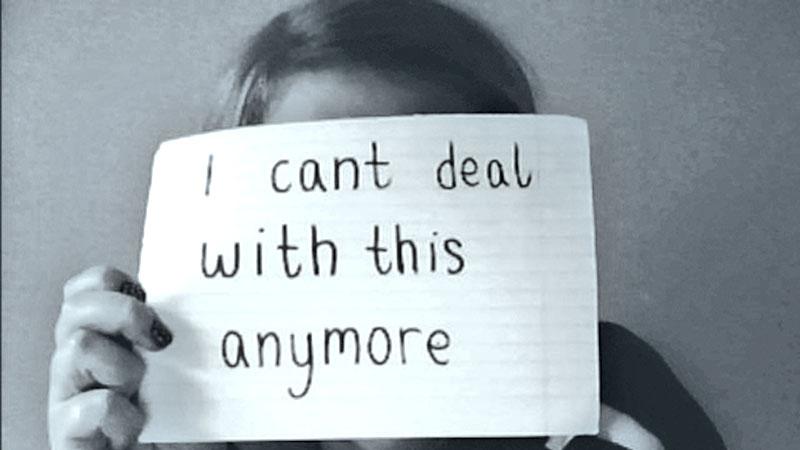
According to him suicide in young people is often a relational process, where they attempt to communicate what cannot be expressed in words. “It can also be a way to express anger, and other taboo emotions such as shame and guilt. Sri Lanka boasts great literacy levels and high-quality education, but in my opinion, we lack emotional literacy, and hence most of us are ill equipped to regulate our emotions. Feelings are not spoken about in most Sri Lankan homes, and expressions of anger, frustration and rage are frowned upon. Suicide in our country, especially, among young people can often be seen as ‘dialogue suicides’ (Marececk, 2006) where the individual attempts to communicate underlying emotions and feelings to others.”
“Dialogue suicides are often directed outside of the self and is often a result of interpersonal strife and struggle. Monologue suicides on the other hand are more oriented inward and are linked to internal despair, loss of hope, and abandonment. The prevalence of dialogue suicides of an impulsive nature among young people are seen to be greater than monologue suicides, although it is known that pre-meditated suicide attempts also take place,” Uduman said.
Young people do reach out to Counsellors, Befrienders, Psychologists and Psychiatrist much more than a few years ago. However, most of these services are available only in the metropolis, and there is limited access to mental health care in rural areas. Young people do not ‘complain’ about their problems to mental health professionals, but they do reach out and that is heartening to note, he said.
Uduman says suicide is a poor coping mechanism in response to a crisis and problems in the lives of young people. “Family dynamics and how crises are seen to be managed at home has a great impact on how young people who observe other family members manage their own problems. Impulsiveness and poor emotional regulation seen in parents has a significant effect on how children cope with difficult circumstances in their lives. The prevailing stigma and shame surrounding mental health problems, and talking about feelings in our country is also an important reason why young people cannot cope with their problems more effectively.”
“Suicide is not a solution for problems and ideally should not be seen as one. There are alternative, healthier coping mechanisms that one can adapt and these must be included in our school curriculum, and even be taught at university level. Young people must be provided with skills to cope with failure, to deal with rejection and manage interpersonal relationships. This is as important as teaching math and science, if not more. Counselling services can also be provided in schools, by adequately trained counsellors who do not double up as teacher-counsellors,” he said.
Awareness
He added that counselling and psychotherapy along with pharmacological interventions sometimes have proven to be very effective in treating depression in both young people and adults. “Awareness is key to the prevention of suicide along with adequate life skills education, beginning at school. There is also a need for the media to engage more in the dissemination of awareness among the masses, and also to engage in ethical and sensitive reporting of mental illness and suicide, in order to prevent copy-cat suicides which have been seen to happen in Sri Lanka. Conversations around emotional health need to happen, and the public also must be provided with basic gatekeeper training on how to recognize and support someone through a suicidal crisis- this could be an effective way to combat the rising number of suicide attempts in the country. There is a role for the government and the health services to play, but also a role for you and me. Suicide prevention is the responsibility of a community, not just mental health professionals,” he said. Clinical Psychiatrist, Government Base Hospital, Psychiatry Unit, Kiribathgoda, Dr. N. Kumaranayake, spoke to the Sunday Observer about depression and its symptoms. He said, “Depression (major depressive disorder) is a common and serious medical illness that negatively affects how you feel, the way you think and how you act. Fortunately, it is also treatable. Depression causes feelings of sadness and/or a loss of interest in activities once enjoyed. It can lead to a variety of emotional and physical problems and can decrease a person’s ability to function at work and at home. Treating depression properly is the main way to prevent suicide.”
Depression symptoms can vary from mild to severe and can include:
- Feeling sad or having a depressed mood
- Loss of interest or pleasure in activities once enjoyed
- Changes in appetite — weight loss or gain unrelated to dieting
- Trouble sleeping or sleeping too much
- Loss of energy or increased fatigue
- Increase in purposeless physical activity (e.g., hand-wringing or pacing) or slowed movements and speech (actions observable by others)
- Feeling worthless or guilty
- Difficulty thinking, concentrating or making decisions
- Thoughts of death or suicide
Dr. N. Kumaranayake said, symptoms must last at least two weeks for a diagnosis of depression. Medical conditions such as thyroid problems, a brain tumor or vitamin deficiency can mimic symptoms of depression so it is important to rule out general medical causes. “Depression is different from Sadness or Grief/Bereavement. The death of a loved one, loss of a job or the ending of a relationship are difficult experiences for a person to endure. It is normal for feelings of sadness or grief to develop in response to such situations. Those experiencing loss often might describe themselves as being “depressed” but being sad is not the same as having depression.
They are also different in important ways:
In grief, painful feelings come in waves, often intermixed with positive memories of the deceased. In major depression, mood and/or interest (pleasure) are on the decline for two weeks.
In grief, self-esteem is usually maintained. In major depression, feelings of worthlessness and self-loathing are common.
For some people, the death of a loved one can bring on major depression. Losing a job or being a victim of a physical assault or a major disaster can lead to depression. When grief and depression co-exist, the grief is more severe and lasts longer than grief without depression. According to Dr. Kumaranayake several factors can play a role in depression. They are Biochemistry, Genetics, Personality and Environmental factors.
Biochemistry: Differences in certain chemicals in the brain may contribute to symptoms of depression.
Genetics: Depression can run in families. For example, if one identical twin has depression, the other has a 70 percent chance of having the illness sometime in life.
Personality: People with low self-esteem, who are easily overwhelmed by stress, or who are generally pessimistic appear to be more likely to experience depression.
Environmental factors: Continuous exposure to violence, neglect, abuse or poverty may make some people more vulnerable to depression.
“Depression is among the most treatable of mental disorders. Between 80 and 90 percent of people with depression eventually respond well to treatment. Almost all patients gain some relief. Before a diagnosis or treatment, a health professional should conduct a thorough diagnostic evaluation, including an interview and possibly a physical examination. In some cases, a blood test might be done to make sure the depression is not due to a medical condition like a thyroid problem. The evaluation is to identify specific symptoms, medical and family history, cultural factors and environmental factors to arrive at a diagnosis and plan a course of action, “Dr. Kumaranayake said. “Medication: Brain chemistry may contribute to an individual’s depression and may factor into their treatment. For this reason, antidepressants might be prescribed to help modify one’s brain chemistry. These medications are not sedatives, “uppers” or tranquilizers. They are not habit-forming. Generally antidepressant medications have no stimulating effect on people not experiencing depression. Antidepressants may produce some improvement within the first week or two of use. Full benefits may not be seen for two to three months. If a patient feels little or no improvement after several weeks, his or her psychiatrist can alter the dose of the medication or add or substitute another antidepressant. In some situations other psychotropic medications may be helpful. It is important to let your doctor know if a medication does not work or if you experience side effects, he said.
“Psychotherapy: Psychotherapy, or “talk therapy,” is sometimes used alone for treatment of mild depression; for moderate to severe depression, psychotherapy is often used along with antidepressant medications. Cognitive behavioral therapy (CBT) has been found to be effective in treating depression. CBT is a form of therapy focused on the present and problem solving. CBT helps a person to recognize distorted thinking and then change behaviors and thinking,” he said. He further said that psychotherapy may involve only the individual, but it can include others. “For example, family or couples therapy can help address issues within these close relationships. Group therapy involves people with similar illnesses. Depending on the severity of the depression, treatment can take a few weeks or much longer. In many cases, significant improvement can be made in 10 to 15 sessions. Unfortunately, Sri Lanka does not have trained counsellors. The school counsellors are not properly trained,” Dr. Kumaranayake said. “If someone indicates they are considering suicide, listen and take their concerns seriously. Don’t be afraid to ask questions about their plans. Let them know you care, and they are not alone. Encourage them to seek help immediately from a knowledgeable professional. Don’t leave them alone,” he said.
Warning signs of suicide
- Often talking or writing about death, dying, or suicide
- Making comments about being hopeless, helpless or worthless
- Expressions of having no reason for living; no sense of purpose in life; saying things like “It would be better if I wasn’t here” or “I want out”
- Increased alcohol and/or drug misuse
- Withdrawal from friends, family and community
- Reckless behaviour or more risky activities, seemingly without thinking
- Dramatic mood changes Talking about feeling trapped or being a burden to others
Counsellors at Attorney General’s offices
Psychiatric Social Workers in most hospitals
Sumithrayo (0112692909)
CCC Line (1333)
