 The World Health Organization in its publication of April 5 2021 commended Sri Lanka’s Health Ministry for the way it ably managed its programme of safeguarding pregnant women, whether infected or not during the Covid 19 pandemic last year, thereby minimising maternal morbidity and mortality.
The World Health Organization in its publication of April 5 2021 commended Sri Lanka’s Health Ministry for the way it ably managed its programme of safeguarding pregnant women, whether infected or not during the Covid 19 pandemic last year, thereby minimising maternal morbidity and mortality.
However, health officials are now faced with new challenges that need to be overcome. For example, although cause-specific deaths related to maternal mortality rates such as haemorrhage, abortion, hypertensive disorders and sepsis have dipped considerably in Sri Lanka due to timely interventions by the Ministry of Health with the support of professional bodies, new challenges continue to mount.
 These include preventing deaths due to heart diseases and pneumonia among pregnant women, the ongoing Covid19 pandemic despite efforts by the health authorities to stop its spread, and the upward trend in unpreventable as well as preventable deaths among pregnant women. Apart from these physical health problems, other factors too have created fresh challenges. The current fuel and transport crisis resulted in delays in seeking early care by pregnant women, while problems in promoting contraceptives to vulnerable women In a sensitive religious and political culture, have also exacerbated these issues. According to reliable information together they are said to account for a sizable increase in the proportion of pregnancy-related deaths last year compared to the previous year.
These include preventing deaths due to heart diseases and pneumonia among pregnant women, the ongoing Covid19 pandemic despite efforts by the health authorities to stop its spread, and the upward trend in unpreventable as well as preventable deaths among pregnant women. Apart from these physical health problems, other factors too have created fresh challenges. The current fuel and transport crisis resulted in delays in seeking early care by pregnant women, while problems in promoting contraceptives to vulnerable women In a sensitive religious and political culture, have also exacerbated these issues. According to reliable information together they are said to account for a sizable increase in the proportion of pregnancy-related deaths last year compared to the previous year.
The Sunday Observer spoke to Consultant Community Physician and National Programme Manager – Maternal and Child Morbidity and Mortality, Dr. Kapila Jayaratne to find out more about these new challenges that impact adversely on pregnant women and most importantly to tell us what strategies there were in place for Lankan mothers to use in order to best overcome them.
Excerpts
 Q: While Sri Lanka has made remarkable strides in lowering its maternal mortality rates winning acclaim from global health authorities including the World Health Organization, maternal mortality rates are apparently stagnating despite efforts to lower them further. Why is this? How does the country rank with other countries in its current MMR rates?
Q: While Sri Lanka has made remarkable strides in lowering its maternal mortality rates winning acclaim from global health authorities including the World Health Organization, maternal mortality rates are apparently stagnating despite efforts to lower them further. Why is this? How does the country rank with other countries in its current MMR rates?
A. Although our maternal mortality rate has been stagnating, our rates are more or less on par with most high income countries and we are well above the general global status.
Q: Sri Lanka’s MMR was reportedly estimated at 36 maternal deaths per 100 000 live births (80 percent UI: 31–41) in 2017. Are the figures still the same as they were three years ago ? .
A. That is an estimation worked out from statistical modelling. We have more accurate and recent data for Sri Lanka. The latest available is for the year 2020; 29 maternal deaths per 100 000 live births. This is interpreted as “when 100 000 babies are born alive, 29 women died of pregnancy-related causes in the year 2020”. In this particular year, the number of maternal deaths was 90 and there were 301 706 live births. This is a remarkable achievement when compared with our neighbouring countries which still struggle to reduce such deaths.
Q: Has the scenario changed now? In what way?
A. Over the years, Sri Lanka has reduced cause-specific deaths in all major disease entities especially haemorrhage, abortion, hypertensive disorders and sepsis. However, now , we are faced with challenges in preventing deaths due to heart diseases and pneumonia. Other factors too have contributed to the rise in MMR. Last year at the height of the pandemic, we experienced a significant number of Covid19 maternal deaths. The proportion of unpreventable deaths is also increasing every year. Delay in seeking care contributes to nearly 50% of dead women. Complex social scenarios linked to some women is a challenge to us. In a sensitive religious and political culture, promoting contraceptives to vulnerable women has become problematic. There is an element of issues in providing quality care too which together have collectively impacted on maternal health.
Q: Sri Lanka was commended as a success story in terms of both reducing maternal mortality and improving its measurement by the WHO in its latest publication of Maternal mortality measurement: guidance to improve national reporting. As a lower middle income country facing many health issues and limited resources, what were the factors that contributed to this success in its long history of caring for pregnant women?
A. A pregnant woman is a precious life in any civilised society and every death of a pregnant woman is a matter of sadness and loss for the whole nation. As a country with high status for women, we started counting maternal deaths far back in the late 19th century. Caring for pregnant women was regularized with the opening of Asia’s 2nd oldest maternity hospital, De Soysa Lying-in-Home in 1879. The maternal and child health (MCH) services were gradually stretched with the launch of an MCH department within the Colombo Municipality. Field MCH services were started in 1906 with the appointment of midwives and the 1st Ante-natal clinic in Asia, for pregnant mothers at De Soysa Lying-in-Home in 1921. The country, perceiving the special status of “two lives” in one body, started reviewing maternal deaths in the year 1959, an initiative only a few countries had adopted by that time. The Maternal Death Surveillance and Response (MDSR) system evolved over the years and was assumed as an active platform to learn from such deaths and implement corrective actions. MDSR contributed to both accurate measurement and reduction of maternal mortality.
 Q: According to the latest WHO guidance report , the case study of the MDSR system in Sri Lanka shows an example of a system that includes mandatory reporting and a clear system of notification and review that addresses the issues in time. What exactly does this mean?
Q: According to the latest WHO guidance report , the case study of the MDSR system in Sri Lanka shows an example of a system that includes mandatory reporting and a clear system of notification and review that addresses the issues in time. What exactly does this mean?
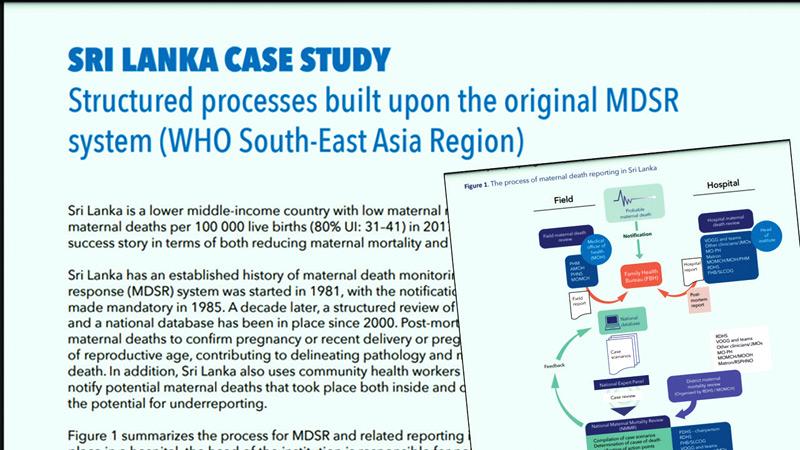
A. It is a mandatory requirement that all responsible officials should notify a probable maternal death; the death of a woman in the reproductive age (15 – 49 years) during the pregnancy period or one year after termination of pregnancy, to the Family Health Bureau (FHB) within 24 hrs. Out of them, true maternal deaths are identified based on the WHO definition; The death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and site of pregnancy, from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes. All these deaths are subjected to a mandatory post-mortem. For each maternal death, field and hospital reviews are conducted and detailed reports with issues, service deficiencies, and suggested actions to prevent them are sent to FHB. A desk review of the cases is done at FHB with the participation of representatives of Sri Lanka College of Obstetricians (SLCOG), public health specialists, anesthesiologists, forensic pathologists, health administrators and other related specialists. A team of health ministry officials and experts then visit each district, present case scenarios, discuss them with district-level healthcare teams, identify issues and work out actions to further prevent such deaths. Implementation of the corrective actions is monitored at multiple tiers in the health system.
Q: I understand that Sri Lanka also uses community health workers (field public health midwives; PHMs) to notify potential maternal deaths that took place both inside and outside of health-care facilities thus minimizing the potential for underreporting. How important is their role?
A. Each household in the country is assigned to a public health midwife. They have registered nearly 3.9 million eligible couples. Again, almost all of the pregnant women in Sri Lanka are registered by PHMs, believe me, 80 percent are before 12 weeks of gestation, and their entire pregnancy, delivery and postpartum care are documented. So they know the outcome of the pregnancy or the fate of the woman. It is the PHM who knows first when such a death happens. She immediately reports it to the medical officer of health (MOH). This is followed by notifying the maternal death to FHB.
Q: Late maternal deaths have been cited as becoming more important as a proportion of total maternal deaths in some countries. What are late maternal deaths ?
A. We take female deaths that happened during pregnancy and up to 42 days postpartum as maternal deaths. However, with the advancement of care, some women suffering from pregnancy-related conditions survive beyond 42 days after delivery and die later. They are termed late maternal deaths; those women who died of pregnancy-related causes between 42 days and one year after the end of pregnancy.
Q: As Community Physician and National Program Manager for the Maternal and Child Mortality Surveillance programme of the Family Health Bureau tell us what role it plays in minimising maternal mortality in Sri Lanka island-wide.
A. We play the central role in executing the MDSR country-wide. Our unit prepares case scenarios, conducts desk and district reviews, and all the minutes following meetings. We send them to all the key agencies and officials who can utilize such information and / or take action. Our team computes national and subnational maternal mortality ratios.
We bring the issues surpassed at death reviews at different higher level policy platforms and facilitate taking preventive actions. We are supported by professional bodies, especially SLCOG and other relevant specialists. Our unit functions under the guidance of Director - Maternal and Child Health, Deputy Director General Public Health Services, Director General of Health Services, and Secretary of Health.
 Q: What are the guidelines that mothers- to- be can follow to prevent complications during or after child birth.?
Q: What are the guidelines that mothers- to- be can follow to prevent complications during or after child birth.?
A. ‘Avoid too early, too late, too many and too frequent’ pregnancies. Better to have your precious baby when you are healthy and between 20 – 35 years of age. Teenage and advanced maternal age pregnancies have more risk of complications. Register your pregnancy early with the area public health midwife. Go for the booking visit. Follow the instructions of your obstetrician. Have a healthy diet. Avoid crowds. Always be prepared for an emergency. Admit to the hospital in time for your delivery. Focus on yourself also after the childbirth. Practice personal safety and hygienic measures all throughout.
Q: What is your message for pregnant women and women who want to be mothers out there ?
A. Better prepared pregnancy is the best preventive strategy. If you are going to get pregnant, be knowledgeable about pregnancy, talk to your area PHM, get advice from your family doctor, participate in pre-pregnancy screening programs and if you have any illnesses consult an obstetrician. If they advise, optimise your body to become pregnant.
Those who are already pregnant, strictly follow advice from PHM, doctors, your obstetrician and other specialists if any. If there is any danger, immediately admit to the nearest government hospital.
Q: Any contact line which a pregnant woman can reach for more information?
A. The best and easily reachable source is the area public health midwife for information. Her contact number is given in the pregnancy record.
The other contact point is the hotline 1999 available 24 hours.
