Cervical Cancer - one of the most understood cancers is still a worrying issue to health specialists treating and researching cancer patients with this condition. Added to their problems is the complex nature of this particular cancer which has led to confusion and wrong beliefs about it among both the patients and their carers.
The Sunday Observer spoke to Consultant Community Physician (Acting) of the National Cancer Control Programme (NCCP) Dr. E.H.K. Fernando to get a more accurate picture of what Cervical cancer is, where it spreads most in the human body, how to detect it and most importantly prevent it at the pre-cancerous stage using available facilities.
Excerpts
Q. Cervical cancer is on the rise both in Sri Lanka and across the world. For our readers benefit tell us what is cervical cancer in laymen’s language. Who are the commonest victims of this disease? From which part of the body does it originate?
 Dr. E.H.K. Fernando |
A. Cervical cancer is one of the commonest cancers among females and a leading cause of cancer deaths among women in the world and also in Sri Lanka. However, over the past 10 - 15 years, this remains static with around 1000 cases being detected annually. It originates from the uterine cervix of the female genital system.
Q. Where is the cervix?
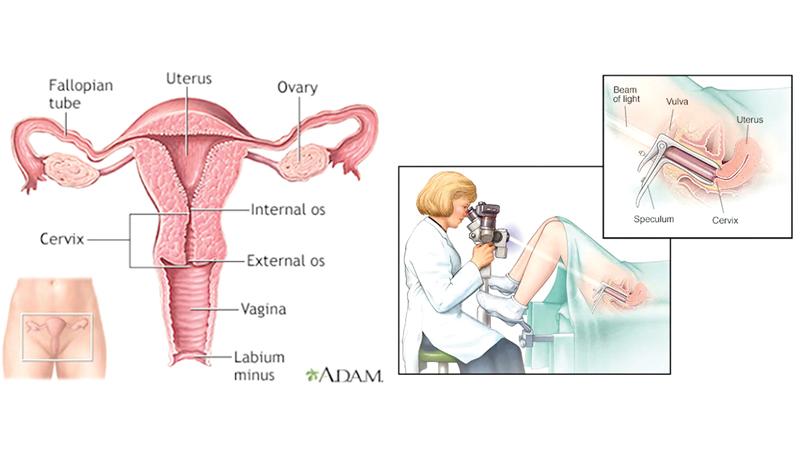
A. The cervix is the elongated opening of the uterus. It opens into the vaginal canal which is situated between urethra and anus. The cervix consists of an ectocervix opening into the vagina and an endocervix opening into the uterine cavity. The ectocervix is covered by the epithelium of the vagina while the endocervix by the uterine epithelium. The junction of these two epithelia is the main area where the cancer originates.
Q. Where does it spread most?
A. Cervical cancer spreads in two main ways.
1. Direct spread to the adjacent organs; rectum, bladder, uterus, pelvic floor
2. Lymphatic spread; To regional lymph nodes, lung, liver and bone.
Q. Are there different types of cervical cancers? If so, what are the most common?
A. Yes, there are two main types of cervical cancers
1. Squamous cell carcinoma (90 percent of the cervical carcinomas) which develops from the squamous epithelium of the ectocervix.
2. Adenocarcinoma
It develops from the columnar epithelium of the endocervix.
Q. Are the symptoms easily detectable to the naked eye? If not why?
A. No. Cervical cancers cannot be detected easily by the naked eye and mostly patients remain asym[ptomatic. Symptoms appear clinically when the cancer is quite developed and spread. Therefore, awareness raising among girls/ women on the causes and risk factors is important for prevention and early detection of cervical cancer as there ways to prevent and detect early.
Q. The National Cancer Registry Data of National Cancer Control Program, has reportedly stated that about 1000 -1200 patients with cervical cancers are newly detected yearly. Do these figures still hold today?
A. Yes. According to the National Cancer registry data in 2019, 1114 new cervical cancer cases were detected in 2019. However, this figure has been stagnant over the last few years.
Q. What are the causes that drive this cancer?
A. The Human Papilloma Virus (HPV) infection is the main cause which is transmitted by sexual activity. HPV types 16 and 18 are the mostly associated virus types.
Also, having multiple sexual partners, early commencement of sexual activities, immunodeficiency, poor nutrition and unhygienic practices are risk factors favouring the development of the infection.
Q. What are the signs to watch out for?
A. 1. Intermenstrual bleeding (Bleeding between regular menstrual cycles. It occurs from a cervical growth)
2. Post-menopausal bleeding (Bleeding after menopause – E.g.: bleeding from a cancerous cervical growth)
3. Post-coital bleeding (Bleeding during or after intercourse – Contact bleeding dueto ulceration of a growth)
4. Anaemia (Due to long term bleeding)
5. Unusual/ smelly vaginal discharges (Due to a growth)
6. Leakage of urine or faeces into vagina (Forming vesico-vaginal and recto-vaginal fistulas)
7. Pelvic, back or leg pain (symptoms of direct spread)
8. Loss of appetite, loss of weight (disseminated spread of cancers)
Q. Is HPV contagious? Can it be treated before it advances thus pre-empting the diseases in its early stages?
A. Yes HPV is contagious. As stated above it is a sexually transmitted disease.
The virus is naturally eliminated by the immune system but in some it is not so.
However, cervical cancer could be prevented/ treated successfully if detected early.
Q. What is the age group most at risk? Under 35 years? At menopause? Elderly women?
A. Girls are exposed to the disease once they start becoming sexually active. However, since this has a prolonged course as it takes around 10 -15 years for the pre-cancerous stage to develop and the pre-cancer to become a cancer. Hence, from the exposure to develop clinical symptoms, it takes a long time.
Q. How is Cervical cancer treated?
A. Cervical cancer is treatable with a combination of surgery, radiotherapy and/or chemotherapy.
Q. Are there vaccinations to prevent it? In some countries schoolgirls are now being vaccinated against some of the most high-risk strains of HPV? .What is the scenario in Sri Lanka?
A. In Sri Lanka too HPV vaccinations are now being given to school girls aged 10-11 (Grade 6) years of age, 2 doses, 6 months apart. The vaccine is given for HPV 16,18(Cancerous types) and 6, 11 (Anogenital warts types) strains.
Q. Can a woman who has been diagnosed with Cervical Cancer have children? If so, will it affect her unborn child?
A. Cervical cancer treatment requires surgery (mostly involving removal of uterus) and also the treatments of radiotherapy which will not permit a woman to have a child after surgery.
Radiotherapy and chemotherapy can have a negative impact on an unborn child.
A mother diagnosed with cervical cancer after pregnancy will be able to deliver the child by cesarean-section. There is no mother to child transmission of the cancer.
Q. If an infected woman has sex with her husband or partner, can she infect her partner?
A. Although Cancer itself is not infectious, Human Papilloma virus is contagious, and can be transmitted to her partner through sexual intercourse.
Q. Prevention – Can wearing condoms protect you from contracting HPV leading to cervical cancer?
A. Yes it can help to minimise the spread.
Q. The World Health Organization (WHO) has declared a ‘Global initiative on elimination of cervical cancer as a public health problem’. The interim targets are (i) Achieve 90 percent coverage of vaccination of HPV vaccine of girls before the age of 15 (ii) Coverage of 70 percent of females at the age of 35 and 45 year using a quality assured cervical cancer screening test (iii) 90 percent comprehensive treatment coverage of females with cervical cancer or pre- cancer. What has the Health Ministry done so far to achieve these targets?
A. 1. Health Ministry has included the HPV vaccination program for schoolgoing girls of 10-11years in the school medical inspection programsince 2017. According to the Epidemiology unit, coverage for the 1st dose was 70 percent and 2nd dose was 51 percent in 2020.
2. Well Women Clinics (WWC) are screening 35y and 45y aged women with PAP smears. Coverage for 35 y age group was 59.1 percent and the 45 y age group was 25.5 percent in 2019.
3. Management guidelines were developed and staff has bee trained. A follow up system is also being developed to monitor the treatment coverage
Q. Are these services free in state hospitals? If so where ?
A. Yes, they are free in all state hospitals, MOH clinics, Well Women Clinics, Cancer early Detection Centres and Sexually Transmitted Diseases clinics islandwide.
Q. Diagnosis and tests- How do you diagnose cervical cancer? Now that we are moving into a new hi tech era, are there easier and more effective methods using new technologies now available?
A. PAP smear test or more advanced HPV DNA test (newly introduced method) is used for screening. Depending on these results, a colposcopy examination will be decided. It is both an investigative plus a treatable procedure for minor lesions.
Q. You mentioned PAP smear. What is a PAP smear?
A. It is a procedure in which a small brush is used to gently remove cells from the surface of the cervix and the area around it so they can be checked under a microscope for cervical cancer or cell changes that may lead to cervical cancer.
Q. If any woman wishes to get more information on this subject, who should she contact?
A. The Area Medical Officer of Health, Midwife, Public Health Nursing Sister in a MOH/ hospital or Cancer Early Detection Centre.
Q. Do you have a message to our readers with regard to reducing their risks of cervical cancer?
A. I wish to reiterate that cervical cancer is essentially preventable/ early detectable and could be successfully treated. My advice is to get the HPV vaccine for girls aged 10 - 11years, and for all women between 35 and 45 to undergo screening for cervical cancer.
