Just three days ago on March 23, chest specialists across the world came together to raise awareness on Tuberculosis (TB) which despite their collective efforts continues to be a global public health concern.
One of the main obstacles in their goal of ending TB has been a reluctance among certain high risk vulnerable groups who are reluctant to get themselves screened for TB even when they present positive symptoms of the disease. This is due to the prevailing prejudices and stigma attached to this contagious, yet preventable disease, largely due to their low health literacy levels that has resulted in many such persons being ignorant of the basic facts about the disease, such as how it is caused, or how it is transmitted.
 Dr. Upul Pathirana |
The Sunday Observer spoke to Consultant Respiratory Physician, District General Hospital and District Chest Clinic Trincomalee and Assistant Editor, Sri Lanka College of Pulmonologists, Dr. Upul Pathirana, to share his expertise on why and how this persistent health problem can be eradicated if not drastically reduced, with resources available free of charge to all patients at district, Provincial and regional level state hospitals.
Excerpts.
Q: For the benefit of readers who are still ignorant of basic facts on TB tell us what is TB?
A. Tuberculosis is an infectious disease commonly caused by a bacteria called Mycobacterium tuberculosis. The organism has the capacity to affect almost all the systems and organs in the human body except a few such as hair and nails.
Q: What is the main mode of transmission of this disease between person to person?
A. person who has the disease in his lungs can release organisms to the environment through their respiratory secretions when he coughs, sneezes or laughs without a protective facemask. This is followed by inhalation of organisms into the lungs of another man who does not have the disease. There is a cascade of reactions once the organism is deposited in lungs. The end result is either he or she can develop the disease or the organism remains inactive within the body, which is called latent tuberculous infection (LTBI).
Q: What are the symptoms that set it apart from other respiratory infections?
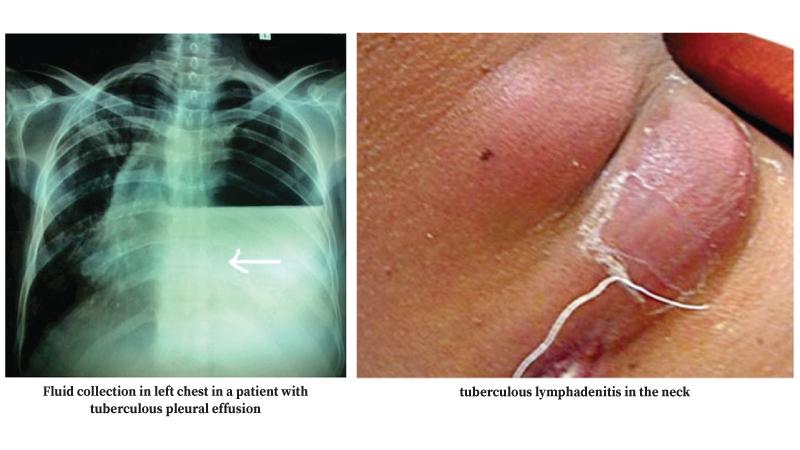
A. We should suspect Tuberculosis in any patient who has a persistent cough for more than 2 weeks. They also can cough out blood in their phlegm. Reduced appetite, loss of weight, night sweats, fever (might be evening fever), chest pain and breathlessness are other common symptoms. Patients can present with symptoms and signs related to the involvement of other sites called extra-pulmonary tuberculosis (EPTB) as well. For example, localised neck swelling due to Tuberculosis affecting lymph nodes.
Q: What is the commonest site for TB in the human body?
A. The commonest site for Tuberculosis is lung, named pulmonary tuberculosis. The organism can spread through the lymphatic system to regional lymph nodes, where we call it tuberculous lymphadenitis. The lungs are entirely encased by two tissue layers called visceral and parietal pleura. The pleura adjacent to the involved lung tissue might be infected with Mycobacterium tuberculosis resulting in fluid accumulation in between visceral and parietal pleura. This is called tuberculous pleural effusion.
A few organisms may disseminate into the distant organs through the bloodstream during the initial exposure and these organisms may remain dormant in lungs and other organs for years without causing the disease. This is defined as the latent tuberculous infection (LTBI). These dormant organisms can reactivate later causing the disease in affected organs such as brain (Tuberculoma), meninges (tuberculous meningitis), joint (tuberculous arthritis), gut (Tuberculous intestine), and any other organ system.
In rare instances, the dissemination through the blood might initiate an active infection involving many sites within the body; the term disseminated tuberculosis is used in this scenario.
Q: How is it diagnosed?
A. Pulmonary tuberculosis is diagnosed by sputum testing and chest X-ray. This is sometimes challenging because we should exclude the other potential causes for their clinical presentation. We also offer advanced radiological investigations such as computed tomography (CT) and Magnetic Resonance Imaging (MRI) where relevant to aid our diagnosis. Tissue sampling for histological examination and microbiological testing will establish a confident diagnosis.
Q: What is Latent Tuberculous Infection( LTBI)?
A. A person infected with Mycobacterium tuberculosis, but without having the disease has LTBI. The bacteria are not active and remain in a dormant form. Therefore, these patients are not symptomatic and they do not spread the infection. The danger of LTBI is the activation of dormant bacteria when our immune system is weak and it initiates the disease process. The Sri Lanka College of Pulmonologists has formulated the guidelines for the evaluation and management of LTBI. They have identified the high-risk group for reactivation and recommend the treatment for LTBI in these categories.
Q: Is it true that HIV infected persons are at highest risk of reactivation?
A. The people living with HIV have reduced immunity and therefore the progression from LTBI to active disease is high in these individuals compared to people without HIV.
 Rheumatologists administer medications, which are necessary to modify the disease activity in some rheumatological disorders. However, some of these medications affect the immune pathway, which protect them from tuberculosis.
Rheumatologists administer medications, which are necessary to modify the disease activity in some rheumatological disorders. However, some of these medications affect the immune pathway, which protect them from tuberculosis.
Therefore, it is essential to look for active tuberculosis and LTBI before initiating such medications. Your rheumatologist will direct you to a pulmonologist for screening of tuberculosis before commencing immunosuppressive treatment that carries a risk of activation of tuberculosis.
Q: Since both Covid-19 and TB are infections of the respiratory system which have a wide clinical presentation, is it possible for an examining physician to confuse the symptoms?
A. Both Tuberculosis and Covid-19 predominantly target the respiratory system even though it is not exclusively confined to it. The disease course is acute in the case of Covid-19 and it is generally subacute or chronic in Tuberculosis. The difficulty arises when both illnesses are coexisting together, where we have to have a high degree of clinical suspicion and offer testing for Tuberculosis in Covid-19 patients and vice versa. However, I must reiterate, that even though the health care demand for the Covid-19 was high over the last 2 years, there was an uninterrupted flow of Tuberculosis services in our country.
Q: Walk us through the initial procedures to detect TB when a patient comes for screening.
A. The medical officer asks about symptoms of Tuberculosis and examines you for physical signs. He will request three samples of sputum to detect the infecting organism by microscopy and you may undergo a chest X-ray as well. Once the initial tests are completed, he may diagnose or rule out Tuberculosis. When the demarcation is not very clear, you will receive an appointment with a Consultant Respiratory Physician.
All the doctors are trained to detect Tuberculosis and therefore, you can ask your doctor whether you need testing and if yes, what tests are required. And also, If anyone wants to screen for Tuberculosis, he/she can directly walk to our district chest clinic (DCC) or outreach centers run by DCC.
Q: Many new techniques have been introduced to detect, and treat patients in this hi-tech age. Are any of these techniques available free of charge in our state hospitals ?
A. Absolutely yes, The gene techniques can give you not only the diagnosis, but also tells quickly whether you have drug resistant Tuberculosis or not. The available techniques are highly sensitive, specific and rapid. These techniques are distributed to cover the whole country and you don’t need to pay for the test.
The test has been introduced recently to the District General Hospital Trincomalee as well. Endobronchial Ultrasound and Transbronchial Needle Aspiration (EBUS-TBNA) is a new development in Sri Lanka and it can sample lymph nodes inside your chest. EBUS-TBNA is available at National Hospital for Respiratory Diseases Welisara, National Hospital of Sri Lanka Colombo and the National Hospital Kandy, and it is free of charge in these government hospitals.
Q: I understand that the Sri Lanka National Programme for Tuberculosis Control and Chest Diseases (NPTCCD) with the support of the Health Ministry has introduced some useful interventions to halt the forward stride of TB. Can you briefly tell us what some of the most recent interventions you have introduced and how successful their outcomes are?
A. Yes. We have a well-organised strong system to detect and treat tuberculosis in Sri Lanka.
 skin tuberculosis |
The National Programme for Tuberculosis Control and Chest Diseases (NPTCCD) is the central organisation of the Ministry of Health responsible for controlling and preventing tuberculosis throughout Sri Lanka. The vision of NPTCCD is “Tuberculosis Free Sri Lanka”. This is achieved by formulation of policies, planning, coordinating and monitoring of Tuberculosis and chest diseases control activities in the country. All these activities are in keeping with World Health Organization (WHO) standards as well.
Each district in the country has a district chest clinic through which Tuberculosis control activities are implemented. The District Tuberculosis Control officer is responsible for the administrative work of the district chest clinic under the technical guidance by the Director, NTPCCD. The clinical activities of almost all the district chest clinics are supervised by Consultant Respiratory Physicians.
Q: Since your vision is “Tuberculosis Free Sri Lanka” what are the gaps you see that hinder the achievement of this commendable goal? Emergence of other infections that can be confused or mistaken for TB especially in those with HIV ? Patients whose health and immune system has already been compromised due to pre existing conditions such as Diabetes? Myth surrounding the disease? Or simply patients not completing their full dosage once they felt better?.
A. HIV patients develop infections by Mycobateria Other Than Tuberculosis (MOTT), which behave somewhat similar to Tuberculosis although there are some differences. Uncontrolled Diabetes mellitus (DM) is a strong risk factor associated with Tuberculosis and they can end up with complications too. Therefore, we want good blood sugar control to prevent and treat the disease successfully and it is important that all patients must complete the full course of treatment to prevent recurrence , as irregular treatment is associated with emergence of drug resistance.
Q: Is there a vaccine to prevent TB? For how long does it offer protection against the disease?
A. Yes. Almost all the newborns are vaccinated with BCG vaccine within 24 hours of birth. The protection offered by BCG is mostly in the initial 5 years of life to prevent complications associated with tuberculosis like central nervous system tuberculosis. It has very minimal effect on adult tuberculosis.
Q: Any words of advice for our readers who may be at risk of being exposed to TB?
A. Tuberculosis is not an inherited (transmitted through generations) disease and anyone of us can catch the infection. If you have had a cough for 2 or more weeks, feel free to come for our assistance.
Early detection and treatment not only prevent lung damage by the disease but also minimise transmitting infection to your loving family. Once the treatment is started the majority are non-infectious.
Therefore, early treatment is the key. You can also help your country to achieve the goal of elimination of Tuberculosis
