Parkinson’s Disease (PD) Awareness week is currently being observed by health officials across the world. The disease which continues to be steeped in superstitions and stigma leading to delays by patients to seek early treatment. Using available resources is the key to help them enjoy a better quality of life, says a neurologist who believes that awareness raising and education of patients is the first step towards halting this world’s fastest neurological condition in its tracks.
The Sunday Observer spoke to Senior Consultant and Neurologist , Sri Jayewardenepura Teaching Hospital Dr Harsha Gunasekera to get a more in depth knowledge about this subject and why he thinks it is so vital to rase more awareness among the Lankan Parkisonian community .
Excerpts.
Q. Starting from April 11- Parkinsonian (Parkinson’s disease) Awareness Raising Month - health officials across the world have begun pooling their ideas and resources on improving the quality of life of patients with Parkinson’s Disease (PD). For the benefit of our readers, could you explain what exactly this disease is?
 Dr Harsha Gunasekera |
A. Parkinson’s disease is caused by a loss of nerve cells in the part of the brain called the “substantia nigra”. Nerve cells in this part of the brain are responsible for producing a chemical called dopamine. Dopamine acts as a messenger (neurotransmitter) between the parts of the brain and nervous system that help control and coordinate body movements (basal ganglia). If these nerve cells die or become damaged, the amount of dopamine in the brain is reduced. This means the part of the brain controlling movement cannot work as well as normal, causing movements to become slow and abnormal.
Q. Why is it necessary to devote an entire month to raise awareness on this specific health topic when there are so many other health problems that require urgent attention right now?
A. Because recent studies have shown that Parkinson’s Disease (PD) is the fastest growing neurological disease globally, with doubling of the number of PD patients over the 25-year period from 1990 – 2015. It’s predicted to double again by 2040. Yet in spite of this, PD is still a misunderstood disease and lack of awareness makes people with PD vulnerable and discriminated against in society.
Q. How common is it in Sri Lanka and how does our prevalence rate compare with other countries according to your latest data?
A. We don’t have national level data to compare with international data. Some clinic studies have shown that classical PD is the commonest type of Parkinsonism in Sri Lanka.
Q. What are the common symptoms associated with it?
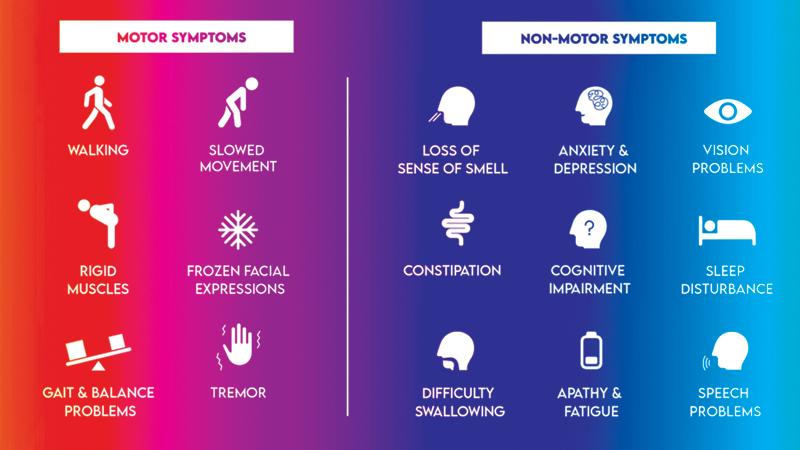
A. “Parkinsonism” is the umbrella term used to describe the common symptom triad of tremor, muscle stiffness or rigidity and slowness of movement. PD is the commonest type of Parkinsonism worldwide. The other movement related (motor) symptoms are poor balance when changing posture, stooping forwards and shuffling when walking, falls, reduced facial expressions (mask like appearance), monotonous speech and small-sized letters with hand writing (micrographia). Its important to understand that PD affects much more than movement. There are over 40 possible “non-movement” symptoms affecting sleep, memory, mood, bowel and bladder control, sexual functions and pain. These distressing symptoms are often invisible and further isolate patients with PD.
Q. Is it curable ?
A. Unfortunately despite ongoing research on this subject no cure for PD has still been found although advancements of treatment can improve quality of life.
Q. What is the special focus of this year’s awareness month for Parkinson’s disease and how relevant is it to Lankans afflicted with this condition?
A. The theme for 2023 Parkinson’s Awareness Month is #Take6forPD, in light of our new incidence study which indicates that a person receives a Parkinson’s disease (PD) diagnosis every six minutes.
Q. Tremors due to advancing age- How does one distinguish symptoms of Parkinson’s Disease from those due to old age tremors?
A. The tremors we see with advancing age are called the senile tremor. This is quite different to the tremors in PD which occur predominantly when the hands are rested (rest tremor) and usually affects one side. Senile tremor affects both hands and occurs when hands are outstretched (postural tremor) or being used for a particular task like holding a cup. Besides this, tremor is a very common symptom which can be seen in a variety of medical conditions which can be differentiated from PD by clinical examination.
Q: Do all those who have Parkinson disease develop the same symptoms?
A. The classic triad of symptoms described above are seen in all patients but may vary in severity and extent. For example, one patient might have a very dominant tremor but less stiffness and slowness or vice versa. The non-movement symptoms also can vary from patient to patient.
 Q. Who are those most vulnerable to developing it age wise and gender wise?
Q. Who are those most vulnerable to developing it age wise and gender wise?
A. PD is indiscriminate against gender, ethnicity, age and geography. Although it’s a neurodegenerative disease most commonly affecting people over 65 years of age, up to 10% of people affected are younger than 40 years.
Q. While it is still unclear what causes Parkinson’s, it has been reported that some cases can be traced to a genetic mutation as well as environmental factors, which coupled with genetics, could play a role in the development of Parkinson’s disease. Do you agree?
A. Yes, the exact cause of PD is still unknown as in most other neurodegenerative diseases such as Alzheimer’s disease and motor neuron disease. A mixture of genetic and environmental factors are thought to play a role in its development. PD can run in families with a faulty genetic mutation but this type of familial PD is very rare.
Q. Brain damage and head traumas -– can they also lead to PD?
A. Head injuries can increase a person’s risk of developing PD. However, even with this increased risk, it’s a very rare complication of head injury.
Q. So if you were to summarise the main underlying causes, what would they be ?
A. Genetic and environmental factors play a role. Environmental factors such as exposure to toxic substances such as pesticides and herbicides, industrial and air pollution may contribute to its development but evidence linking PD to environmental factors has been inconclusive.
There are several causes for secondary Parkinsonism which includes long term use of certain medications, following stroke and some brain infections.
Q. Is PD a slow process or does it happen overnight?
A. The loss of nerve cells in the brain is a slow process and it predates the onset of symptoms by a number of years. The symptoms appear only after 50% of the nerve cell activity in the area of the brain called “substantia nigra” is lost.
Q. How can it be diagnosed ? What are the tools you use ?
A. Diagnosis of PD is essentially clinical based on the patient’s symptoms and signs. In rare instances, doctors may use brain scans to rule out other secondary causes and other disease states.
Q. Who is able to diagnose it ?
A. For the initial diagnosis, it’s better to refer the patient to a neurologist or a specialist physician as important decisions need to be made on initiation of treatment. Movement disorder clinics are established in some major hospitals for these patients to be followed up.
Q. Once a patient has been diagnosed with Parkinson’s disease what is the next step? Take us through the procedure followed.
A. Specific treatment measures are directed at increasing the dopamine levels in the areas of the brain affected by the disease. Initially, patients may have only mild symptoms, which may not affect their functional status. However, these patients need treatment using the appropriate first line treatments (usually oral medications). Later on, as the disease progresses treatment may need changes. In addition, physiotherapy for improving mobility and balance and speech therapy in patients with swallowing difficulties will be recommended as appropriate. All patients should be assessed and provided general and supportive care for non-movement symptoms which are distressing but invisible.
Q. Does a patient have to be warded once diagnosed? Or can he/she be treated at home?
A. No. Most patients are assessed and initiated on treatment as outpatients. The initial first line treatments are decided depending on the severity of symptoms and the age of the patients.
Q. How effective and safe are these treatments?
A. The current treatments available are effective in controlling symptoms and improving the quality of life of patients. They are relatively safe. However, as the disease progresses usually beyond 3 to 5 years, patients may notice a reduced response and fluctuations in their response to the treatments. When this occurs, appropriate advice should be taken from the neurologist to minimise these changes. Under any circumstances, the treatment should NOT be stopped abruptly as this can lead to a serious complication called the “acute dopamine withdrawal syndrome”.
Q. Any new breakthroughs in diagnosis, and treatment interventions?
A. New treatment formulations to deliver the medications to the intestine or to the circulation using an infusion pump are available in some developed countries. In addition, in selected patients who are not controlled on optimum medications are recommended surgical treatment or deep brain stimulation.
Q. Are they available in Sri Lanka as well?.
A. Unfortunately not.
Q. I understand there is an Association of Sri Lankan Neurologists (ASN) which is in overall charge of such patients. What has this Association done so far to raise awareness on PD and ensure a better quality of life for both the patients and their carers?
A. ASN together with the Movement Disorder Society of Sri Lanka (MDSSL) conducts educational programs to update health professionals on advances in the management of patients. Awareness programs are conducted, especially connected to World Brain Health Day activities to promote brain health among the public.
Q. Your message to patients?
A. A diagnosis of PD is life changing. Long term treatment will be needed to control the symptoms and with time you may need to adapt changes to your lifestyle even to the extent of changing the way you do simple activities of daily living. The medications prescribed should be taken carefully and at no time should be stopped abruptly. Regular exercise helps PD patients to reduce muscle stiffness, improve mood and relieve stress.
Q. Is there a hashtag or website that can be reached by persons wanting more information on this subject?
A. The International Parkinson and Movement Disorder Society has resources available for patients which can be downloaded at; 5https://www.movementdisorders.org/MDS/Resources/Patient-Education.htm
