 This year’s theme for Breastfeeding Week which begins on August 1 could not have come at a better time. Today new factors have emerged to escalate the already existing problems of the Lankan nursing mother such as rising costs of living, shortages of vital medicines, increased prices on many prescription drugs, constant strikes by hospital staff- all of which have added to their stress levels and sidelined the priority they should give to their health and the likely adverse effects on their foetus. Added to this we also have an ongoing Covid-19 and Dengue crisis and likelihood of pregnant mothers being exposed to these infections.
This year’s theme for Breastfeeding Week which begins on August 1 could not have come at a better time. Today new factors have emerged to escalate the already existing problems of the Lankan nursing mother such as rising costs of living, shortages of vital medicines, increased prices on many prescription drugs, constant strikes by hospital staff- all of which have added to their stress levels and sidelined the priority they should give to their health and the likely adverse effects on their foetus. Added to this we also have an ongoing Covid-19 and Dengue crisis and likelihood of pregnant mothers being exposed to these infections.
So how do we close these gaps that prevent quality care reaching Lankan mothers across the country irrespective of nationality, education status or religion? The Sunday Observer sought answers to these questions from an eminent Neonatologist Dr. Nishani Lucas, Senior Lecturer at the Department of Paediatrics, University of Colombo and Consultant Neonatologist University unit, De Soysa Hospital for Women Colombo.
Q: This year’s theme for breastfeeding week which begins on August 1 is “closing the gap: breastfeeding support for all “. Why was this specific theme chosen when most mothers breastfeed their babies anyway, at least in developing countries like ours?

Dr. Nishani Lucas
A. The annual theme for the breastfeeding week is chosen by the World Alliance for Breastfeeding Action (WABA). Although more than 82 percent of Sri Lankan infants were breastfed according to 2016 data, only 44 percent of infants were exclusively breastfed globally from 2015-2020.
Q: The theme refers to gaps that need to be closed. What exactly are these gaps?
A. The gaps are situational challenges that need to be overcome by mothers in order to successfully breastfeed their babies. These include working away from home, unavailability of paid maternity leave for 6 months duration, inadequate skilled support for breastfeeding due to poorly trained health workers, inadequate support from family members as well as from society, lack of protection from marketing formula milk that undermine the confidence in breastfeeding as well as various myths and misunderstandings that lead mothers to believe that they do not have adequate breast milk for their baby or that the main reason for babies’ crying is in inadequate breast milk.
Q: So how do breastfeeding activists hope to fill these gaps?
A. Increasing awareness among mothers, their families as well as society about these gaps and methods to overcome them, strengthen breastfeeding counselling training of healthcare workers, and advocacy.
Q: Can all mothers breastfeed?
A. Yes, all mothers can breastfeed. There are only very few exceptions; Mothers who are on chemotherapy or radiotherapy as part of cancer treatment are advised not to breastfeed. However, mothers on any other drugs or therapies can usually breastfeed. Another contraindication to breastfeeding includes a critically ill mother whose clinical condition deteriorates with breastfeeding. These mothers can resume breastfeeding when their clinical condition improves.
Q: What about mothers with pre existing conditions like diabetes or heart problems?
A. There are no medical conditions in mothers that prevent breastfeeding, with the exception of mothers with severe heart disease where the clinical condition deteriorates with the act of breastfeeding due to a very weak heart function (very low ejection fraction), which is a very rare phenomenon. Breastfeeding is particularly beneficial for babies of mothers with diabetes, as breastfeeding decreases the insulin requirement in the mother as well as decreases the risk of transmission of diabetes to the baby.
Q: There are many myths surrounding breastfeeding that continue to persist despite the high literacy rate among women in Sri Lanka. From your own experience as a neonatologist what would you say are the most common?

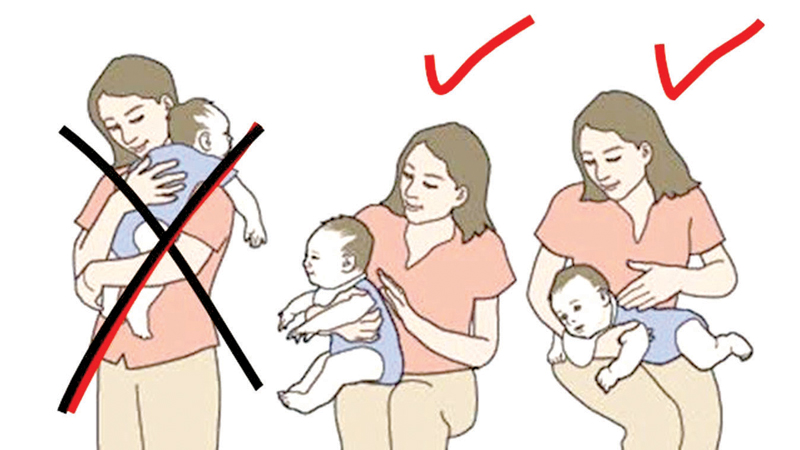
How to hold the baby – 1
A. The most common myths are that ‘most mothers don’t make enough milk for their babies’, ‘most common reason for babies crying is inadequate breast milk’, ‘feed the baby every 2-3 hours’ and ‘feed the baby for at least 20 minutes’.
Q: Does the size of the breast matter when breastfeeding? Some women believe that small breasts or over large breasts could interfere with feeding their infant with enough milk. Do you agree?
A. The size of the breast does not affect breastfeeding at all. The size of the breast depends on the amount of fatty tissue within the breast compared to the number of alveoli, which are responsible for breast milk production. A large breast is due to increased fatty tissue and does not result in the production of more milk. A large breast is associated with more challenges towards breastfeeding compared to a smaller breast which makes it easier to breastfeed.
Q: Some mothers are reluctant to breastfeed as they are afraid their breasts would sag.Your comments?
A. Unfortunately, this is yet another myth. It is not breastfeeding that causes the breast to sag, but inadequate support for the lactating breast. Breast size increases with increased milk production. Cooper ligaments which support the breast, tend to stretch with increase in breast size. Supporting these ligaments to prevent them being overstretched or being damaged, is vital in maintaining a good breast shape and preventing sagging. This new and increased breast size should be firmly supported, by wearing a well-fitting brassire. This will ensure good support for the ligaments supporting the breast.
Q: A disturbing trend now on the rise is that many working mothers, especially those who wish to return to work earlier than the six months advocated by UNICEF and WHO for fear they may be replaced by their employers on grounds of profit loss, are switching to formula feeding. Is there any way to stop this? If so, how? Storing and freezing their milk till they return? How does she do this?
A. Yes, this is one of the main gaps identified. Increasing awareness about the importance of breastfeeding and its lifelong effect, as well as the harms of formula feeding and its detrimental lifelong effects i.e. increased risk of cancer, obesity, diabetes, hypertension, coronary artery disease in baby with formula feeding, would be a key aspect in empowering women to make the right decision. All women should be aware about their right to maternity leave, its duration, as well as the right to have breastfeeding breaks. Expression of breast milk manually is an essential skill that should be learnt by mothers who are returning to work. Return to work should be planned, while gradually arming oneself by building a store of expressed breast milk about 2 weeks prior to having to return to work.
Expressed breast milk should be given via cup and not from a bottle, as suckling from a bottle teat confuses the baby with suckling from the breast and increases the chance of the baby stopping breastfeeding. In addition, using a bottle increases the risk of the baby getting an infection due to the Difficulties in cleaning the feeding bottle. If the mother is away from home for long periods and the baby starts to lose weight or has poor weight gain due to inadequate volumes of expressed breast milk, the baby should be started on complementary feeding instead of formula milk once the baby completes 4 months of age.
Q: How long will expressed milk be kept in the freezer? At what temperature should it be kept?
A. Expressed milk can be kept in the freezer at 00F or -180C for up to 6 months.
Q: Many new mothers also have concerns about how best to hold the baby while feeding. Could you tell them how this should be done and what position the baby should be held in order to ensure he/she gets sufficient milk?

How to hold the baby – 2
A. The baby should be supported along the back, by having his / her head and neck in the same line. The baby’s head should be supported by the mother by supporting the nape of the neck instead of pressing on the back of the baby’s head. This allows the baby to move away if there is a risk of suffocation. Pressing on the back of the head does not allow this freedom and hence increases the risk of suffocation. The baby should be held as close as possible to the mother with the whole baby facing towards the mother. Baby’s head can be supported by the mother’s palm or the mother’s elbow.
Q: Most newborn babies have a windy problem. Is it due to incorrect burping?
A. Yes it is due to incorrect burping. Holding the baby upright is not an effective burping technique, especially if done by a woman. This is due to the lack of a hard surface to compress against the baby’s tummy which is full of air. Keeping the baby on his / her tummy and pressing gently on his/her back for about 10-15 minutes helps the baby to get rid of most of the air that has been swallowed.
Q: Do fathers have a role to play in supporting their wives to breastfeed? How?
A. Of course, fathers have a very important role in supporting their partners to breastfeed. Keeping the mother happy and confident is a key aspect in attaining success in breastfeeding. Not blaming the mother, as well as preventing others from blaming the mother for challenges in breastfeeding, or weight loss in the baby is a very important aspect in building confidence in the mother to aid breastfeeding. In addition, fathers can help around the house to ease the stress of housework in addition to the challenges of breastfeeding, yet again playing a vital role in achieving successful breastfeeding.
Q: As many mothers are still unaware of the benefits of breastfeeding compared to bottle feeding, can you list some of the most significant benefits for both mother and baby?
A. Benefits for the baby include, increase in brain volume as well as improved function, through increase in the synaptic connections as well as increase in myelin. Breast Milk protects the baby against respiratory (72 percent less), diarrhoeal (64 percent less) and ear (50 percent less) infections and reduces the risk of sudden infant death (38 percent less). Breast milk reduces the risk of leukemia (1.2-1.3 fold), malocclusion (68 percent less) as well as allergic conditions like asthma, eczema and allergic rhinitis in the baby. It also reduces the risk of obesity (26 percent less), diabetes (27-39 percent less), hypertension, hypercholesterolaemia and coronary artery disease in the baby in adulthood, through changes in the microbiome as well as epi-genetics. Benefits for the mother include reduced risk of breast, ovarian and uterine cancer, less depression and anaemia, better bone health, increased bonding with baby as well as faster weight loss to regain her pre pregnant physique.
Q: So when should a mother start breastfeeding? As soon as the baby is born or later? Why?
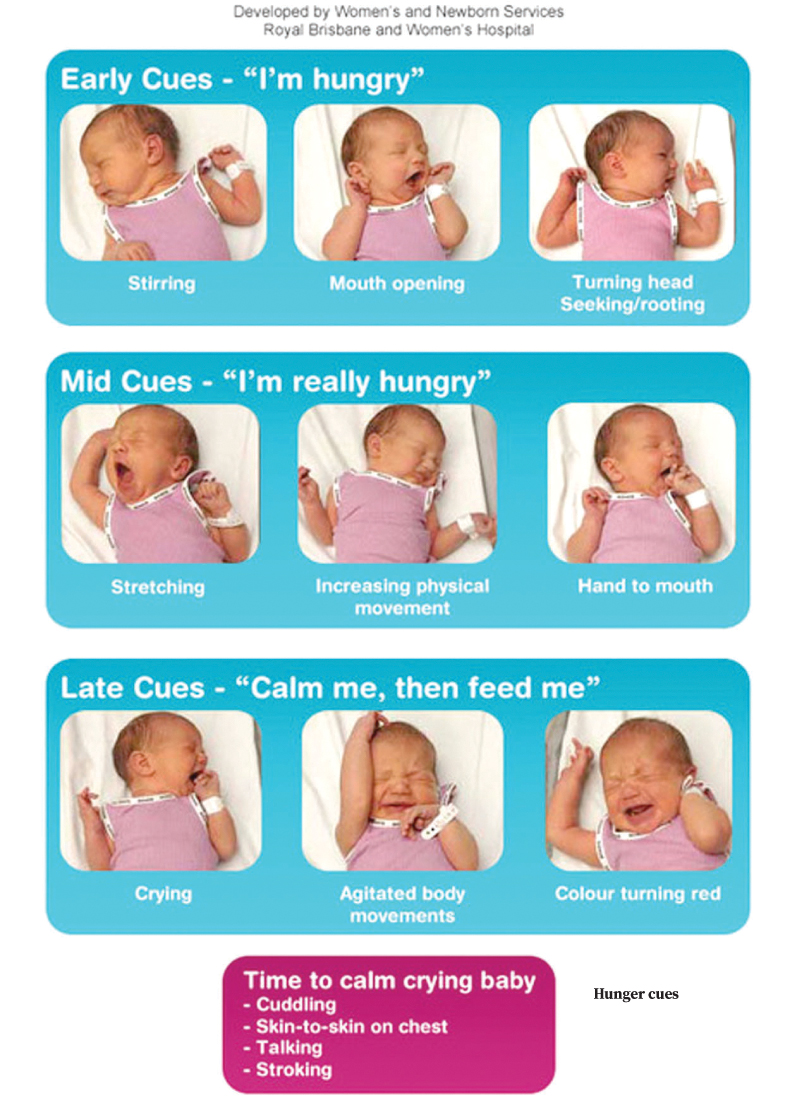
A. Mothers should start breastfeeding as soon as the baby is born and the baby indicates that he / she is hungry i.e., displays hunger cues (opening mouth, looking around to feed, putting hands in the mouth, sucking on the hands.) Studies have shown that giving the first breastfeed soon after birth, as soon as the baby first displays hunger cues, within the first hour of life sets precedence for subsequent successful breastfeeding, as well as higher rates of exclusive breastfeeding.
Q: Some mothers throw away the first drops of thin milk. But I’m told this is the best milk as it prevents infection and bacteria. Do you agree?
A. Yes, I completely agree. The first drops of milk, known as colostrum, is not white in colour and may not typically look like milk. However, it contains a large amount of protein including immune protective substances that are vital in protecting the baby against infection caused by bacteria, virus, fungi as well as protozoa. Therefore, these first drops of milk are considered as the golden elixir of life and should definitely not be discarded but fed to the baby.
Q: Any message for new mothers out there ?
A. All mothers can breastfeed, but it may not come naturally to everyone. Therefore, demand for skilled breastfeeding support and do not accept prescription of formula, unless your life is in danger due to breastfeeding. Prescribing formula milk takes only a few seconds but supporting breastfeeding takes a lot of time and patience. Beware of healthcare workers prescribing formulas, to seek higher profit, as they don’t want to spend time on you. You are subjecting your baby to a lifetime of suffering. Seek help from your public health midwife or go to the nearest lactation management centre (LMC) to get the help you need.