 With Dengue Fever raging across the country and the number of confirmed cases and fatalities rising at an alarming rate, the Sunday Observer spoke to Consultant Virologist and Head, Department of Virology, Medical Research Institute (MRI) Dr. Janaki Abeynayake to find out how the disease is transmitted and to share with us some basic, easy- to- follow rules on how all of us as a nation, can minimise the risks of this most preventable and treatable disease simply by keeping our neighbourhood clean and our own gardens free of utensils and objects that attract the Dengue carrying vector.
With Dengue Fever raging across the country and the number of confirmed cases and fatalities rising at an alarming rate, the Sunday Observer spoke to Consultant Virologist and Head, Department of Virology, Medical Research Institute (MRI) Dr. Janaki Abeynayake to find out how the disease is transmitted and to share with us some basic, easy- to- follow rules on how all of us as a nation, can minimise the risks of this most preventable and treatable disease simply by keeping our neighbourhood clean and our own gardens free of utensils and objects that attract the Dengue carrying vector.
Excerpts
Q: Dengue Fever (DF) is currently raging across Sri Lanka, raising alarm bells among all those closely involved with or looking after persons vulnerable to dengue risks. While many of our readers now know the basic facts about DF due to ongoing education and awareness programmes by the Dengue control Unit and Health Ministry, many are still ignorant of the basic facts regarding the disease. For their benefit, could you explain what DF is?
Q: Is it vector-borne or caused by a bacteria?

Dr. Janaki Abeynayake
A. Dengue fever (DF) is a viral vector borne disease. There are four different closely-related Dengue virus (DV) types. Dengue infection (DI) can be caused by any of the four DV types.Thus, individuals can be infected with DV multiple times in their life. Vectors are Aedes species mosquitoes. It is not a bacterium.
Q: How does it spread and how is it transmitted?
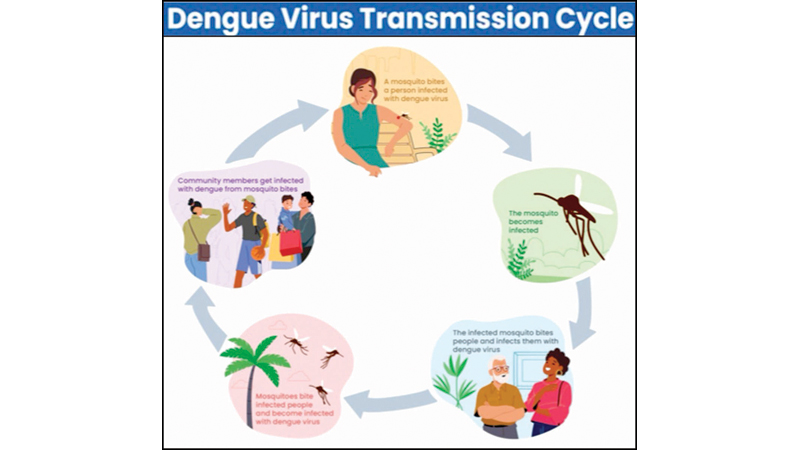
A. DV usually spreads to humans through bites of infected Aedes species mosquitoes, and the main mode of transmission is following an infected mosquito bite.
Q: Is it contagious? How?
A. No, it is not contagious. It is not possible to spread the DV from one individual to another by direct contact. DV typically enters a person after a bite of an infected mosquito. It means, to transmit the virus from an infected person to an uninfected person, a relevant mosquito vector is essential to carry the virus.
Q: What is the name of the mosquito that is responsible for transmitting the disease?
A. Aedes aegypti/Aedes albopictus are the primary vectors that carry/spread the DV, active in early morning, after sunrise and late afternoon before sunset; live both indoors as well as outdoors near people, only females mosquitoes bite humans.
Q: How can it be identified among non DF transmitting mosquitoes to indicate it as the DF carrying mosquito? Are there specific identification marks on its body?
A. The mosquito vector of DV can be identified with the distinctive markings; in Aedes aegypti white markings on its legs, a lyre-shaped pattern on the thorax, in Aedes albopictus striped legs, a more robust body ictus.
Mosquitoes infected with DV, after biting an infected person. Even though direct/visual identification of DV carrying mosquitoes is challenging, it can be identified through specific laboratory test methods.
Q: I understand there are four serotypes of the virus that mainly cause DF. True or false?If so, what are they?
A. True, there are 4 DV serotypes namely dengue-1, dengue-2, dengue-3, and dengue-4.
Q: How many of them are circulating in Sri Lanka right now?
A. Basically, right now there are 2 dengue serotypes circulating. Those are dengue-2 and 3 with dengue-3 predominating. Dengue-4 is occasionally reported as sporadic-cases.
Q: Are there levels of severity in the way they impact on the human body- such as from mild to moderate to severe?
A. Generally studies have not demonstrated dengue serotype-specific differences in clinical manifestations. Some studies show no differences in the fulfilment of WHO-2009 warning signs, though there were significant serotype specific differences on haematological parameters, and plasma viral-RNA-levels; after adjusting for age, and primary/secondary infection status.
Q: What is the worst form of DF?
A. While many DI are asymptomatic or produce only mild illness, viruses can occasionally cause more severe disease, even death. DHF is a more severe form of DF that can be life-threatening. This condition can lead to dengue shock syndrome (DSS), a critical state requiring immediate medical attention.
Q: How do you recognise symptoms of DHF?
A. Those who are infected for the second time are at greater risk of DHF. Symptoms includehigh fever (40°C). Typical DHF symptoms often come after the fever subsides. It is characterised by severe abdominal pain, fatigue, ecchymosis/purpura, bleeding gums, nose, vomiting, blood in vomit or stool, hematuria, rapid breathing, restlessness, postural hypotension. Laboratory findings can demonstrate progressive increase in hematocrit and low platelet count.
Q: What is the difference between DHF and DF?
 A. Following 5–7 days after an infected mosquito bite, DF begins with mild or no symptoms. Early clinical findings are nonspecific with flu-like symptoms. DF may include fever 2–7 days.Other signs/symptoms may include severe headache, retro-orbital pain, myalgia and arthralgia, maculopapular rash. Majority of DF patients will recover in 1–2 weeks. Some DF patients progress to a severe condition called DHF. Warning signs of progression to DHF usually occur around defervescence. DHF includes the symptoms described above.
A. Following 5–7 days after an infected mosquito bite, DF begins with mild or no symptoms. Early clinical findings are nonspecific with flu-like symptoms. DF may include fever 2–7 days.Other signs/symptoms may include severe headache, retro-orbital pain, myalgia and arthralgia, maculopapular rash. Majority of DF patients will recover in 1–2 weeks. Some DF patients progress to a severe condition called DHF. Warning signs of progression to DHF usually occur around defervescence. DHF includes the symptoms described above.
Q: Can Dengue Fever be mistaken for any other disease with similar symptoms like the viral flu?
A. DF can indeed be mistaken for other diseases present with similar symptoms, particularly viral infections like flu. It’s initial clinical presentation is very similar to other mosquito-borne viruses like ZIKA, chikungunya, and should be carefully monitored until dengue is excluded. In tropical countries, possibly elsewhere, DF confuse with other common tropical infections like enteric-fever, leptospirosis, typhus-fever, malaria, and hanta-fever.
Q: What is the latest data you have on suspected cases and dengue deaths?
A. Currently we are experiencing dengue type 1 and 2 circulating in the community and adults are mostly affected.
In some patients dual infections are evident infecting with both dengue type2 and 3. Our present data indicates that almost all provinces have reported cases with the highest numbers being reported in the Western province. Generally, deaths are very minimal.
Q: If a mother-to- be gets dengue, can it affect her unborn child? How?
A. Data are limited on health outcomes of dengue in pregnancy and effects of maternal infection on the developing fetus.
DVI has been associated with a higher risk for abortion if infection occurs during the first trimester, as well as a higher risk for low-weight and preterm birth. Vertical transmission could be considered for mothers who are symptomatic late in pregnancy or at delivery.
Q: Is there a cure for Dengue Fever?
A. Yes, of course. Dengue should be identified early. People should seek medical advice on time. In DF, described as symptomatic, supportive management would recover patients within 1-2 weeks. In severe dengue, hospitalisation at the correct time and close monitoring of intake/output, vital signs and other appropriate treatment could help recover dengue patients.
Q: Can it be reversed if the disease slows down if early medical advice is sought ?
A. Yes. This is important to emphasise that medical advice is very important in DI management. One fact is, DF should be controlled only with specific anti-pyretics. The other fact is dehydration should be managed appropriately. Accurate fluid balance maintenance is very important. Prevent dehydration with plenty of fluids other than water and monitor vital signs of dehydration carefully, because overload of fluid and electrolytes imbalance would harm the patient. This could be done as in-patient or out-patient management under medical guidance after medical advice.
Q: Treatment wise, how is DF treated?
A. There is no specific antiviral for dengue. The focus is on symptomatic treatment. Acetaminophen/paracetamol is often used to control pain. Non-steroidal anti-inflammatory drugs like ibuprofen/aspirin are avoided as they can increase the risk of bleeding. DF patients should take rest, drink adequate fluids and maintain a nutritious diet. Antibiotics do not help. Depending on the clinical manifestations patients might need only ambulatory care or with severe dengue may often require hospitalisation. Pregnant women with dengue should always be hospitalised.
Q: Is it a blanket treatment for all patients or tailored according to the age, health status etc of the patient?
A. The management is generally tailored to patients according to their symptoms and examination findings. Risk factors for DHF include a person’s age, immune status, as well as co-morbiditiesare given special attention with close monitoring, appropriate supportive care. Types of infecting DV should also be given greater attention, because individuals who were previously infected with another DV type are thought to be at greater risk for developing DHF if infected from another dengue type.
Q: Who makes the final diagnosis on whether or not a patient has DF?
A. Apart from the clinical diagnosis DI can be confirmed by specific different laboratory test methods, with different levels of accuracy/sensitivity.According to patient presentation, test should be offered.These tests should be conducted in reliable laboratories with quality control measures.Clinical interpretation and patient clinical history co-relation should be done by a Medical specialist.
Q: How is DF diagnosed? Does the patient have to be hospitalised afterwards or can he or she go home immediately afterwards?
A. Early stage diagnosis tests include antigen-detection and viral-RNA diagnosis. Positive test confirmed DI.Viral-RNA-detection test can differentiate the infected dengue-type. During the later stage;day 5 of illness or after patient presentation, antibody-detection tests are useful to detect DV infected patients.
Hospitalisation of dengue patients should be assessed individually. The decision will be made after considering the stage and the clinical presentation of the patient. Medical experts can make recommendations and guidance after thorough evaluation, to manage the patient either inward or outward.
Q: I understand there are guidelines on Do’s and Don’ts regarding DF in general and DHS. Share them with our readers please.
A. Don’ts
* Do not prescribe aspirin/ibuprofen or corticosteroids routinely.
* Avoid giving IV fluids unless the patient is bleeding/haematocrit level is rising. *Avoid blood-transfusion unless the haematocrit is falling dangerously or platelet transfusion unless the platelet count is very low/unless there is bleeding.
Remember to practise:
* Teach patients: about warning signs, tell out-patients when to return, how to recognise critical phase which begins with defervescence or an increasing haematocrit, to closely monitor fluid intake/output, vital signs, and hematocrit levels, to recognise and treat early shock which characterised by increasing heart rate, delayed capillary refill or cool extremities.
* Patients suspected of suffering from DHF or DSS should be hospitalised without delay, reviewed regularly at 1–2 hour intervals, and monitor platelet counts and haematocrits frequently. * Determine correct timing to give intravenous-fluids. Report all suspected/probable dengue cases to health authorities.
Q: How do you prevent Dengue risk factoes (DRF) starting from community level upwards?
A. Prevention of dengue is based on control/minimise of vector breedings inside/homes. Every household can undertake simple measures to prevent breeding by draining-out water from various containers, regularly changing water, cleaning flower vases, other items or, in the case of unused items, by discarding/destroying those. Mosquitoes cannot travel far, thus, “house cleaning” of a community will ensure no breeding places, and prevent dengue transmission.
Other than dengue surveillance activities in high risk areas, using laboratory methods such as molecular epidemiology could predict next outbreaks,risk geography and relevant dengue type/strain. This would help to adopt/implement preventive/control public health strategies in-advance.
Q: Finally your advice to the public in general regarding minimising DF risks in the future given the new technology we now have with us.
A. The best approach for minimising DF risks is to break the transmission chain by mosquito control/preventive activities widely through community engagement and application on personal protective methods to avoid mosquito contract. Early case notification to the relevant Medical-Officer-of-Health in the area to take immediate control/preventive measures to minimise the case-load, reduce morbidity/mortality in the country.
Q: Is there a hotline or website for anyone to reach for more information?
A. Yes. 011 79 66 366 is now active daily from 8 am to 8 pm.