In today’s medical practice the focus on the holistic/comprehensive care of the individual (as opposed to the patient) has become subservient to attempting to treat/manage illness in patients. The concept of preserving good health by incorporating and practising preventive and curative aspects of medicine to achieve physical, mental and social well-being in individuals, families and communities by medical professionals adhering to the highest possible standards of professional ethical conduct seems to be a utopian ideal instead of a practical day-to-day reality. There are numerous reasons for not being able to achieve this desired state, but the problem is that over time, Sri Lanka seems to be moving away from this ideal rapidly. We as doctors are forgetting why patients come to us. We are imposing our ‘superior’ knowledge and skills on patients more often than not in an unsolicited manner. In short, we have developed and come to accept as normal, a system of doctor-centred care in which a medical condition/disease has become the fundamental issue needing the doctor’s attention. We have lost the art of focusing on the holistic health needs of patients. A minuscule amount of these health needs will definitely require addressing medical conditions/diseases. This is why we need to shift our focus on patients now, more than ever.
 I shall analyse the past and present of the Sri Lankan health system and attempt to answer the following questions and lay out a few proposals for change and how I see the SLMA’s role in such changes.
I shall analyse the past and present of the Sri Lankan health system and attempt to answer the following questions and lay out a few proposals for change and how I see the SLMA’s role in such changes.
Why do we need to shift focus from disease to patients?Why do we need to begin now?
Sri Lanka over the past 100 years has transformed in terms of demography and epidemiology. Sri Lanka has the highest aging population in the world and 1.7 million persons will be added to the elderly cohort during the next 15 years. Relative contribution from mortality due to Non-Communicable Disease (NCD) which is currently very high (80.7%), is projected to remain high by 2030 (81.8%). Furthermore 35% of Disease Adjusted Life Years (DALYs) in Sri Lanka in 2015 was from 3 risk factors – poor diet, uncontrolled blood pressure and uncontrolled blood sugar and more than 50% of the risk factors contributing towards DALYs in 2015 were found to be amenable to behaviour interventions/changes. What data shows is that risk factors which contribute to the highest morbidity and mortailiy in Sri Lanka are not disease-specific but are patient-specific, requiring patient-specific general measures rather than disease-specific interventions.
Sri Lanka is said to have a health care facility within 3.6 km of a household which delivers free health care at the point of delivery. The question we in the health system should be asking is, What should these free healthcare facilities and the staff in them be doing to improve the individual/family and community health status in a rapidly changing society with increased expectations of quality care in terms of personalized care?
Overview of Healthcare System.
Particular attention should be drawn to the 830 Healthy Lifestyle Centres, 500 Primary Care Units (PMCUs) and 354 MoH Units spread throughout Sri Lanka
These are the points of delivery of Primary Ambulatory Curative and Primary Preventive Care. The Healthy Life Centres and PMCUs are severely under-utilized due to poor quality of care they currently offer leading to the ‘by-passing phenomenon’. As summarized in Table 3 the state hospital based Out-Patient Departments (OPD) accounted for 54,652,070 patient encounter episodes in 2015. The overwhelming majority of these visits were primary ambulatory curative care visits, which do not require secondary/tertiary hospital based ambulatory care. In these settings the focus of attention should be the patients rather than the diseases in terms of screening for NCDs and treating minor health issues and referring patients to higher levels of care for ‘disease–specific’ health interventions and follow-up if needed.
Out of Pocket Expenditure (OOPE) on Health
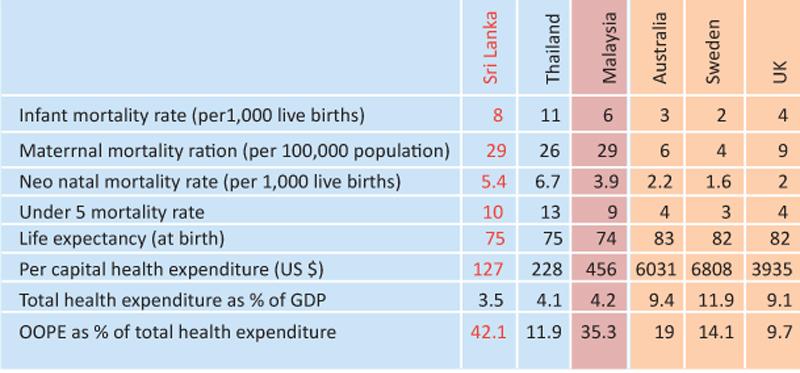
A comparison of Sri Lanka’s health status internationally is given in Table 4. Most of the health indicators are on par with developed countries. But, what is alarming is that Sri Lanka is having a high OOPE on health (42.1%). This is of concern and given the demographic, epidemiological and health consumption/utilization patterns, has the potential to push vulnerable sections of society into catastrophic health spending. This ironically is taking place in a state sponsored health care system supposed to be free at the point of delivery!!!
 According to the Household Income and Expenditure Survey (HIES) of 2012/13 the average OOPE for health ranges from Rs 213.88 to Rs 7,323.68 with a mean of Rs 1,488.28 per month for the total sample. For households, which incurred any health expenditure during the study period, the OOPE for health ranged from Rs 609.16 to Rs 9,419.44 with a mean of Rs 2,557.03 per month. Taking the OOPE per household as Rs 1,488.28 per month the total OOPE for Sri Lanka in 2012/3 was Rs 96 billion (excluding other indirect cost such as transport, cost of ‘by standers’ etc. etc.).
According to the Household Income and Expenditure Survey (HIES) of 2012/13 the average OOPE for health ranges from Rs 213.88 to Rs 7,323.68 with a mean of Rs 1,488.28 per month for the total sample. For households, which incurred any health expenditure during the study period, the OOPE for health ranged from Rs 609.16 to Rs 9,419.44 with a mean of Rs 2,557.03 per month. Taking the OOPE per household as Rs 1,488.28 per month the total OOPE for Sri Lanka in 2012/3 was Rs 96 billion (excluding other indirect cost such as transport, cost of ‘by standers’ etc. etc.).
Analysis of the HIES in terms of specific disease and population groups is given in Table 5. It shows that if a household has a member suffering from a chronic disease and who is elderly that household will have catastrophic health spending which is going to push them into poverty as a direct result of out-of-pocket health spending. With increasing elderly population and the persons with NCDs the average OOPE on health will show an exponential increase in the coming decades, further aggravating the problem of impoverishing healthcare.
In this context ‘Has Sri Lanka got health system mechanisms in place to provide services to match the current and future healthcare consumption needs of our population?
In the 7 decades since independence what we have done is:
We as a health system have essentially concentrated and achieved ‘development’ of Tertiary and Secondary Health Care services. – In Quantity and to some extent in Quality mainly in the State Sector we have achieved Primary Preventive Care service delivery in terms of both, Quantity and Quality, exclusively in the State Sector. This constitutes the foundation of our excellent basic Health Statistics.
More importantly in the 7 decades since independence what we have not done is concentrate on the development of Primary Ambulatory Curative Care Services, both, in terms of quantity and quality in the state and private sectors.
A quick review shows that we have come to be very good at treating disease – eliminating polio, malaria and control of communicable diseases to a point that these no longer are a major cause of mortality across the age groups. We seem to be measuring the health status of our population based on the presence or absences of disease and infirmity. – IMR, MMR, rates of hospital admission, number of ‘cases’ of a specific disease. The number of disease-based health indicators we get are based on number of patients who decide to seek ‘treatment’ from a healthcare facility geared to ‘treat’ illness (as opposed to facilities predominantly focused on preserving health while also treating ‘illness’) (Fig: 1)We seem to have little emphasis on ‘wellbeing’ of the population as a health indicator and even less emphasis on ‘taking care of the whole person’ in our healthcare system.
A conceptual framework for what needs to be done:
Need to shift from the concept of identifying, understanding and managing health from one of ‘absence of diseases’ to one which identifies, understands and manages health from a perspective of ‘wellbeing’
Need to shift from measuring disease as health to measuring wellbeing as health
Need to address these health issues within and without the health system in patient centred manner.
The application, implementation and practice of the Universal Health Care (UHC) in a sustainable manner within the Sri Lankan health system will allow today’s vision of shifting focus from diseases to patients to become tomorrow’s reality.
Role of a national medical association in this process
Set up mechanisms to
i. Address provision of UHC through patient centred healthcare (Please see Fig 3)
- Development of essential service package for primary – same healthcare at Primary Medical Care Unit (PMCU) settings for all
- Development of technical guidelines for patient referral pathways for holistic healthcare – Rational heath care delivery guaranteeing Universal Health Care (UHC)
- Development of staffing needs based on workload as opposed to staffing needs based on cadre requirements – Guaranteeing quality care
ii. Create awareness and introduce healthcare innovations
- Make the shift from evidence generation to innovations and development in health care setting up a Healthcare Innovations and Practices Hub (SLMA-HIPH) at the SLMA
Develop partnerships to increase access to healthcare
i. Between system – Primary/Secondary/Tertiary and between Western and Traditional systems
ii. Between public and private sectors. Advocate at all levels for:
i. Patient centred, integrated healthcare delivery system
ii. Team based care addressing whole spectrum of patient needs
Through these developments the SLMA with other local and international partners would envisage that the next decade or more in the Sri Lankan health sector development will be dedicated to development of Primary Ambulatory Curative Care.
We from the SLMA call upon all stakeholders to join us in calling on the government to declare the next decade as THE DECADE OF PRIMARY CURATIVE CARE.
