 The focus for this year’s World Physiotherapy Day which fell on September 8 was on low back pain (LBP) and the role of physiotherapy in its management and prevention.
The focus for this year’s World Physiotherapy Day which fell on September 8 was on low back pain (LBP) and the role of physiotherapy in its management and prevention.
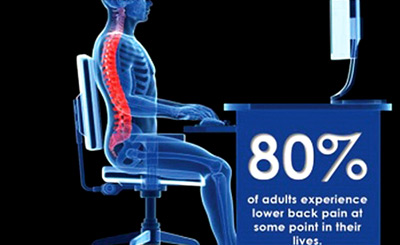
According to the research statistics 619 million people experienced LBP in 2020. Physiotherapists provide expert advice, guidance and treatment for LBP. It is advised that non-surgical treatments be used to support LBP sufferers. Physiotherapists are experts in treating lower back pain (LBP) and many provide a customised treatment plan in that scenario.
Based on clinical experiences and recent research studies, low back pain affects approximately 1 in 13 people, making it a significant global health issue. Clinical Practice Guidelines (CPGs) recommend that physiotherapy should be a first-line treatment for low back pain, particularly in the absence of serious underlying conditions. The combination of education, exercise, manual therapy, and self-management strategies is often endorsed based on evidence supporting their effectiveness in managing low back pain and improving functional outcomes.
Low back pain can be categorised in various ways based on its duration, origin, and specific characteristics
Acute Low Back Pain: This endures for a few days to a few weeks. It frequently happens after strain or injury, including moving suddenly, lifting a big object, or adopting an unnatural posture.
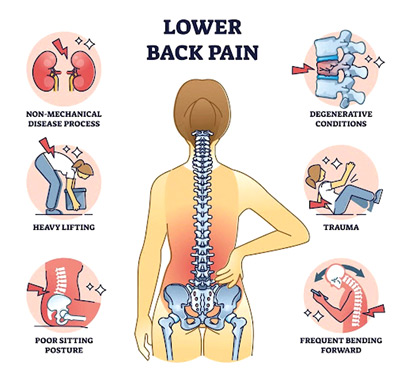 Chronic Low Back Pain: For longer than 3 months, this continues. It may develop spontaneously or as a persistent, intense pain. Conditions including degenerative disc disease, arthritis, or prior injuries may cause chronic pain.
Chronic Low Back Pain: For longer than 3 months, this continues. It may develop spontaneously or as a persistent, intense pain. Conditions including degenerative disc disease, arthritis, or prior injuries may cause chronic pain.
Subacute Low Back Pain: This type of pain lasts for 4 to 12 weeks and is in between acute and chronic pain. Conservative treatment usually cures it.
Mechanical Back Pain: This is related to the structure of the spine and surrounding muscles. This pain is typically worsened by movement and resting usually makes it better.
Radicular pain: Also known as sciatica, is frequently brought on by a herniated disc or spinal stenosis compressing a nerve and causes pain that radiates down the leg as a result of irritation on the nerve root.
Referred Pain: This pain is felt in the lower back but originated from another area of the body, such as kidney or pelvis.
Non-Specific Low Back Pain: This is the most common type and doesn’t have a clear, identifiable cause.
Specific Low Back Pain: This is associated with identifiable causes like fractures, infections, tumours or other medical conditions affecting the spine.
Inflammatory Back pain: Inflammatory arthritis can cause this type of pain, characterised by stiffness and inflammation.
Role of Physiotherapy in Low Back pain
 Physiotherapy plays a multifaceted role in managing low back pain, from initial education and pain relief to long-term functional rehabilitation and prevention. Selecting the right course of therapy and management techniques for low back pain can be aided by knowing the type of pain. It’s critical to get medical assistance for a comprehensive evaluation if the pain is severe, chronic or accompanied by other symptoms like numbness, weakness or loss of control over bodily functions.
Physiotherapy plays a multifaceted role in managing low back pain, from initial education and pain relief to long-term functional rehabilitation and prevention. Selecting the right course of therapy and management techniques for low back pain can be aided by knowing the type of pain. It’s critical to get medical assistance for a comprehensive evaluation if the pain is severe, chronic or accompanied by other symptoms like numbness, weakness or loss of control over bodily functions.
1. Patient education and self management (sitting, standing, walking, driving, sleeping position advice)
2. Exercise therapy includes strengthening, stretching, and tailored exercises to specific issues
3. Manual therapy techniques includes spinal manipulation, mobilisation
4. Functional training and rehabilitation to improve mobility, strength and endurance with bio mechanics
5. Behavioural and cognitive approaches to pain education, relaxation and mindfulness
6. Long term management and prevention with ergonomic adjustment and encouraging ongoing exercise
7. Modalities may be used to complement exercise therapy
After conducting a thorough assessment of the patient, the physiotherapist can develop a tailored treatment plan based on the patient’s specific needs. Proper assessment should includes following key components;
Patient history and pain assessment
Physical examination, posture analysis, range of motion testing and functional assessment
Perform special tests to differentiate the proper diagnosis
Plan the treatment with short-term and long-term goals
 If a proper assessment is not conducted, the treatment may not be effective, leading to unsatisfactory outcomes for both the patient and the therapist. To achieve at least 95% satisfaction, it is crucial that both the patient and the physical therapist actively participate in the assessment and treatment process. This collaborative approach ensures that the treatment plan is well-informed and tailored to the patient’s specific needs, enhancing the likelihood of a successful outcome.
If a proper assessment is not conducted, the treatment may not be effective, leading to unsatisfactory outcomes for both the patient and the therapist. To achieve at least 95% satisfaction, it is crucial that both the patient and the physical therapist actively participate in the assessment and treatment process. This collaborative approach ensures that the treatment plan is well-informed and tailored to the patient’s specific needs, enhancing the likelihood of a successful outcome.
Therefore, schedule your appointment with a professional service and consult your physiotherapist in advance to determine which type of treatment is safe for you.







