“I follow the great teachings of the Buddha, Yōgilānanupatteiya sō maņ upatteeiya - those who tend to the sick, tend to me’. This is the low tech - high touch technique of providing community palliative care,” says Dr. Samadhi Rajapaksa.
“With my long experience in community palliative care, I would say one has to start something even in a small way with least resources. It depends on one’s inspiration and determination. Next is unity, for which we have proven evidence; together each achieves more. Being compassionate and authoritative helps one to approach patients, family members and the civil society. Our technique is physical and moral courage, which is very effective for sustainability. None of these things belong to high tech, but to high touch.”
Palliative care never says “there’s nothing we can do.” It is about living as well as dying. It is an essential human right of each person affected with terminal illness to receive proper palliative care wherever they live.
It is a prime duty of every healthcare person to put into practice palliative care as needed by the terminally ill.
It is an area where relieving and preventing the suffering of patients are taken into consideration. The WHO defines palliative care as “an approach that improves the quality of life of patients and their families facing the problem associated with life threatening illnesses through prevention and relief of the suffering by means of early identification, impeccable assessment and treatment of pain and other problems, physical, psychological or spiritual”.
Research findings reveal that palliative care can improve the quality of life, at times survival of patients with life limiting illnesses. With the rapid increase of population and the consequences of epidemiologic transition to enlarge life limiting diseases, there is an immense need for palliative care development. Unfortunately, one-third of the world population with terminal illness has no access to palliative care.
The management of pain and other symptoms and provision of psychological, social and spiritual support is paramount. Palliative care services can be developed in many different settings, hospital, home, hospice, outpatient clinic, local health centre, mobile clinic or in a daycare centre.
In 2003, as an intern medical officer attached to the teaching hospital of Anuradhapura, Dr. Samadhi Rajapaksa, realised that there was an immense need to develop palliative care service in Sri Lanka.
During this time palliative care services were limited, and knowledge as well as interest was inadequate even among medical professionals.
Although the facilities available were insufficient, his determination was strong within the limited resources. Dr. Rajapaksa started a clinic with the concept, ‘Savimath Manasin Ikman Suwaya’ - Speedy recovery through strong mind, with the blessings of the Consultant Oncologist at that time.
Thus palliative care clinics were conducted once a week for cancer patients who deserved care. It was the beginning! “My aim was to uplift their psychological, social and spiritual standards. Within two years 383 patients benefited through this clinic.” he said.
“Though palliative care should be everyone’s concern, obtaining community support for this worthy cause was difficult,” he said. In 2003, Dr. Rajapaksa, started the Cancer Care Association of Sri Lanka (CCASL) registered under the Social Service Registry, in the Anuradhapura district.
The patients were provided counselling and psychological support by the CCASL, conducting religious activities such as mindful meditation, pirith chanting and Bodhi pooja.
As the tertiary care unit in Anuradhapura was overcrowded, the need of a hospice was felt and discussed with the authorities. The message was passed to the community through several awareness programs.
A patient who came to his clinic offered to donate two acres of land to establish a hospice. A hat collection made, walking from Anuradhapura to Kandy for five days helped the initial construction work.
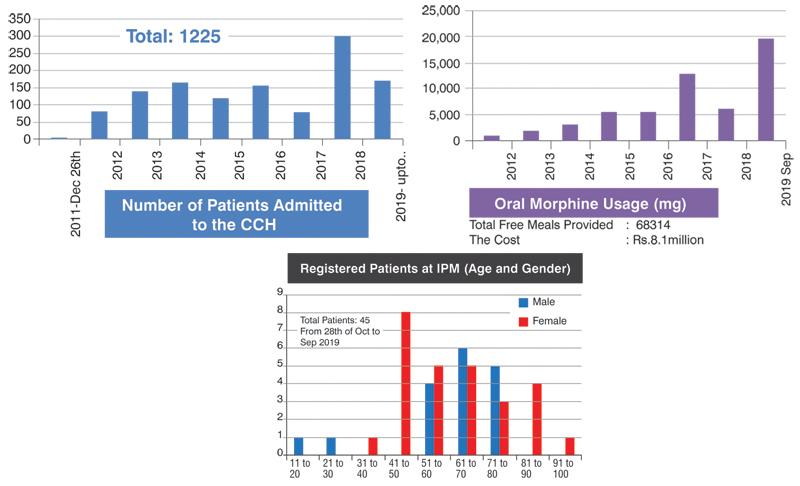
At present the hospice at Kurundakulama, Anuradhapura, has the capacity for 46 beds which cost $0.3 million. It involved a lot of hard work and effort, and the first patient was admitted on December 26, 2011.
The WHO donated 22 beds. The hospice is registered under the Private Health Services Regulatory Council. The CCA provides trained healthcare workers, counselling, low stress activities and social support.
Total Morphine Use up to now: 56,419mg
The CCASL has now set up its branches in Colombo, Galle and Matara. Sensitisation programs on palliative care are conducted at these centres, and more than 5,000 life members are actively engaged in voluntary service.
The Blooming Flower Program of the CCASL supports children’s education in instances where the breadwinner of the family is a terminally ill cancer patient. Upto now 460 educational scholarships have been offered.
The Institute of Palliative Medicine, situated in Nupe, Matara is the first institute dedicated for palliative medicine in Sri Lanka.
Patients by their Diagnosis – Malignant/ Non- Malignant
Home based palliative care is beneficial to those with advanced complex illnesses or life-limiting diagnoses and high risk of morbidity and mortality. This service can increase the standards of care and symptom control, and is cost effective. Most people choose to die at home if there is a good supportive service and high quality care.
The CCASL initiated the ‘Home based Palliative Care Service’ for the needy, terminally ill patients free of charge in 2011 with the minimum facilities. The care givers used public and personal transportation to visit patients in their homes, walking many miles.
They visited patients in rural areas where the infrastructure was minimal, carrying medicine and other necessary stuff on their shoulders.
The capable, caring voluntary Home Care Team of CCASL includes medical officers, nursing staff, counsellors, social workers, helpers, and on special request physiotherapist, nutritionist and clergy. The medical officer and the nursing staff take care of the patients’ physical needs.
Highly interactive and encouraged care givers strictly monitor the physical, mental, social, and spiritual well-being of patients and their family members.
“Sri Lanka’s health policy has not been comprehensive to support and establish community palliative care. Lack of expertise and experienced health care professionals in the field is a big hindrance. Poor attentiveness on palliative care, non availability of drugs, financial difficulty, cultural barriers and difficulty in finding volunteers are other obstacles.
Therefore, it is important that the Government gives due recognition to organisations and those engaged in palliative care to encourage them to involve in such work and make their contribution.
It is vital that the government includes palliative care in medical discipline and develop palliative care specialists to widen and improve the field of palliative care.” Dr. Samadhi Rajapaksa said.
