A global killer, Stroke, more than most other diseases, claims millions of lives each year, the numbers tripling for every decade after 46 years, research has shown. Recently published facts show that 1 in 6 persons will have a stroke or brain attack in his/her lifetime. Globally, stroke is the world’s 3rd leading cause of death after heart disease and cancer, and the commonest cause for adult disability.
 Risk factors for stroke have taken a sharp upward turn in recent years with the rise of non communicable diseases, such as, hypertension, diabetes, high cholesterol, lack of exercise, stress, alcohol, smoking and of course the fast paced life that a competitive society has thrust on us.
Risk factors for stroke have taken a sharp upward turn in recent years with the rise of non communicable diseases, such as, hypertension, diabetes, high cholesterol, lack of exercise, stress, alcohol, smoking and of course the fast paced life that a competitive society has thrust on us.
Stroke has been described in many terms but none so chilling as a‘ silent killer’ which even though the patient may not be aware of, could cause damage to the brain tissue. This brain attack can vary from mild to severe and patients have just a few hours to get life saving treatment.
“The sooner they are diagnosed, and treated , the earlier will be their recovery”, says, Senior Consultant Neurologist, Sri Jayawardenepura General Hospital and President National Stroke Association of Sri Lanka, Dr Harsha Gunasekara.
In an interview with the Sunday Observer, Dr Gunasekara tells readers why it is important to pay attention to the smallest signs and symptoms that indicate the onset of a stroke, which is now the second leading cause for hospital deaths and urges relatives of stroke victims to rush the patient to a hospital, ideally with a stroke unit where he/she can be cared for by a multi disciplinary team to help maximize improvements.
Excerpts…
Q. What is the current stroke burden in Sri Lanka? Can you give any insights from the recently released Sri Lanka Stroke Clinical Registry Data?
A. National Data on stroke incidence in Sri Lanka is not available. Two studies carried out at community level suggest that every year more than 1% of our populationdevelop stroke – that means 200,000 stroke victims annually. Sri Lanka Stroke Clinical Registry has given important facts on Stroke in Sri Lanka in hospitalized patients. The results were based on data collected over a six month period from 5 teaching hospitals in the country.
The salient findings were that 57 % of strokes occurred in males and one third of patients were less than 60 years of age, still in the productive age of their lives. 7% of stroke occurred in people less than 45 years. Although the time taken from the onset of stroke to reach the hospital is critical for recovery following the stroke, only 16% of patients had reached the hospital within 3 hours of symptom onset. Only 3% of patients had received thrombolytic medication (clot buster treatment).
Q. What are the main reasons for stroke in relatively younger age groups?
A. Risk factors for stroke and other non-communicable diseases such as heart disease and cancer are quite similar. In a majority of these younger patients, the same risk factors that cause stroke in the elderly play a role.
This means people are acquiring conditions like high blood pressure, diabetes, high cholesterol levels and heart disease at a relatively younger age. Only a minority of young stroke patients have other rare disease states that predispose them to stroke.
Q. What is the best way to prevent a stroke?
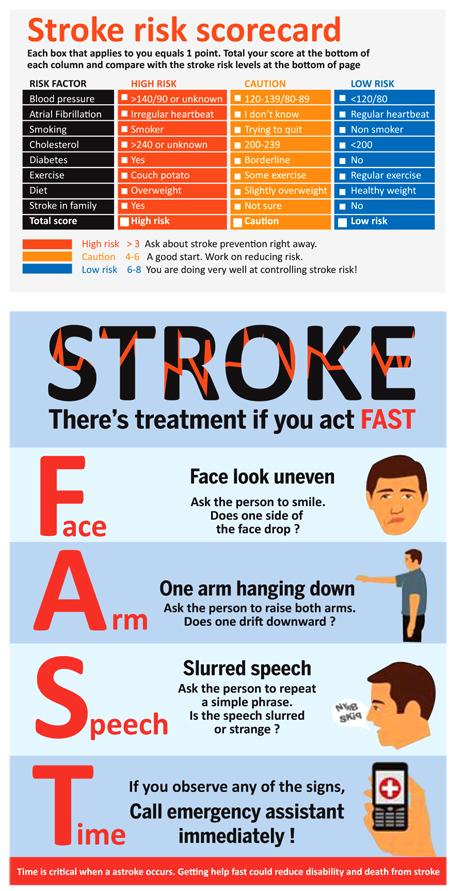
A. The first step is to know your own personal stroke risk. This can be assessed using a simple risk assessment chart seen below. The World Stroke Organization has also put out an easy to use App called Stroke Riskometer available free of charge to download. Once you know your risk, the next step is to identify risk factors applicable to you and take corrective measures.
According to the World Stroke Organization data, 90 % of stroke that occur are linked to 10 key risk factors. They are high blood pressure, smoking, diabetes, high blood cholesterol, irregular heart rhythm, lack of physical exercise, unhealthy diet, obesity, heavy alcohol consumption and lack of awareness about stroke.
The important fact is that all of these risk factors are totally controllable. The initial screening for risk factors will need a consultation with a doctor and some basic tests.
Q. And after that?
A. Continue to carry on the advice given on how to control your risk factors. These will include adaptation of a healthy lifestyle and if necessary some medications. Easiest steps in maintaining a healthy lifestyle is to avoid both, active and passive smoking and take alcohol in moderation (2 units a day for men and 1 unit a day for women). Next is to maintain a normal body mass index (18.5 – 24.9) and healthy waist circumference (less than 40 inches for men and 35 inches for women).
Even with a normal BMI, a raised waist circumference increases your risk of stroke. Regular moderate physical exercise (e.g. walking) for 30 minutes a day for at least 5 days a week is recommended by most professional bodies.
Regular exercise together with healthy (in terms of both quality and quantity) balanced diet – rich in fibre, fruits and vegetables and low in saturated fats, salt and sugar helps maintain a healthy weight. Get your blood pressure, blood glucose and cholesterol levels checked and take treatment if advised by your doctor. Controlling your risk factors before developing a stroke (also called primary prevention) reduces your lifetime stroke risk by 80%.
Q. A common misconception is to confuse a stroke with a heart attack. Is stroke the cause of heart attacks or vice versa?
A. Stroke is a “brain attack” and occurs due to either the clogging of a blood vessel to prevent blood from reaching the brain, or due to rupture of a blood vessel in or near the brain. A heart attack is when blood flow to the heart is interrupted causing damage to the heart muscle.
The symptoms of stroke are very different to the commonly understood symptoms of heart attack. It is essential to be aware of both and respond immediately.
Stroke does not cause heart attacks, but due to the similarity of causative risk factors, a person with a stroke has a higher risk of developing a heart attack. Heart attacks can give rise to stroke, especially, in the early stages, due to the development of blood clots within the diseased heart that can become mobile and clog a blood vessel leading to the brain.
Q. What are the early symptoms of stroke? How do you recognize them?
A. Knowing the “FAST” recognition of signs of stroke is the best way to remember the commonest signs of stroke (see diagram). If any of the 3 signs are positive, the patient should be taken to the nearest hospital immediately.
Around a quarter of patients with stroke may experience a Transient Ischaemic Attack (TIA or mini Stroke). Here the symptoms of stroke last only a few minutes and then rapidly resolve.
This condition should be given serious consideration and treatment initiated immediately as it may be the only warning one may get before developing a major stroke.
Action must be taken early – rush to the nearest major hospital – not the general practitioner next door.Stroke Units are available in all teaching hospitals and most provincial general hospitals.
Q. What should NOT be done till help arrives?
A. The brain is very sensitive to the lack of oxygen and glucose and can only survive between 3 to 5 minutes without them; brain health is time – so act fast.
Do NOT put food or water into the mouth of the patient, and do not sit them up as this could increase the risk of choking.
Instead, turn them on their side and tilt the head back to open the airway and prevent them choking on their tongue, especially, if they are unconscious. When the patient attempts to communicate and if they have difficulty in talking, make suggestions to allow easier communication. The severity of the stroke can vary, so symptoms may settle and improve after a while. However, a stroke has still been experienced – so rush to hospital.
Q. Why is it so important to take the patient to hospital immediately?
A. The patient suspected to have developed a stroke should be taken to the nearest major hospital. When you look at the Stroke clinical registry data, only 16 % of patients arrived at the hospital within 3 hours which is the time limit to administer clot buster injection.
The reasons for this could be lack of awareness of Stroke signs or absence of pain in stroke. Most patients with a heart attack rapidly seek treatment because of severe pain in the chest and receive life saving treatment. Even if there is no pain, Stroke should be considered as a “Brain Attack” and the patient brought to the closest major hospital.
Q. At the hospital, what is the first line of treatment?
A. The patient will undergo a quick clinical assessment to confirm the Stroke signs and then subjected to CT scan which helps in identifying the type of stroke (a brain bleed or blockage of a blood vessel ). Clot busting treatment will be given to eligible patients after assessment. All patients are assessed for any abnormality in blood pressure, oxygen and glucose levels and corrected if necessary. These factors affect stroke of any type adversely.
All patients with stroke will also be assessed and treated for possible complications such as infections (of the lungs and the urinary passage), DVT (clots in the leg veins), pressure ulcers and depression, which would adversely affect recovery.
Q. Rehabilitating victims? How do you get about this difficult task? Who is responsible ?
A. Rehabilitation of a stroke victim requires multidisciplinary support and is best undertaken in the setting of a Stroke Unit. A Stroke Unit in a hospital may be a separate section or part of a ward that cares for stroke patients exclusively.
The stroke unit is composed of: Doctors dedicated in treating patients, Nurses who oversee skin care, oral hygiene, bladder and bowel care and nutrition and general overall care for patients, Physiotherapists who oversee breathing and chest movements, help in regaining motion of limbs and preventing contractures, Speech and Language therapists – assess and manage swallowing difficulties and provide speech exercises, helping communication skills gradually resurface again, Occupational therapiststo help the patients adapt to activities of daily living and Psychological and socioeconomic support through counsellors and social workers. It has been proven that treatment in a Stroke Unit improves chances of survival and reduces both, disability and length of hospital stay.
Q. What are the ‘golden’ rules to follow after a stroke?
A. Once you suffer a stroke, your risk of a second stroke increases significantly. Stroke clinical registry data shows 18% of patients had recurrent Stroke. Therefore, carefully continue all medications prescribed and maintain healthy lifestyle to prevent another stroke (this is called secondary prevention). Even after suffering a stroke or a TIA, if you adopt preventive measures, you can still bring down your risk of having another stroke by 40%.
Q. What about exercise after a Stroke ?
A. Guidelines for exercise recommend increased moderate aerobic physical activity for 150 minutes a week (i.e. 30 minutes a day for 5 days). There is no limitation to the type of aerobic physical activity as long as the patient can cope with it safely (especially with the aim of avoiding falls). After recovery from Stroke, exercise could be started gradually with the help and guidance of the physiotherapist.
Q. What is the current status of care for Stroke victims in Sri Lanka? Any new developments?
A. Stroke services in Sri Lanka over the last 10- 15 years have improved from a minimum level care to essential stroke care services with the establishment of stroke units in hospitals and availability of clot busting treatment. Sri Lanka should now look at improving to a level of advanced stroke care with state-of-the-art treatment techniques such as, clot evacuation, intra-arterial treatment etc.
The proposed National Stroke Hospital at Mulleriyawa is a major step taken towards achieving this goal. Possibility of developing Stroke as a Sub Specialty and train specialists for exclusive care of Stroke patients is currently being looked at. Considering rehabilitation of stroke victims, stroke units are established in most teaching and provincial general hospitals. Training of Rehabilitation Specialists is currently underway.
